The long road to a Covid-19 vaccine | Free to read
It was hailed as a breakthrough vaccine for dengue fever, a neglected tropical disease that kills about 20,000 people each year. Dengvaxia, made by Sanofi Pasteur, was being rolled out to more than 800,000 schoolchildren in the Philippines when reports began trickling in of vaccinated children falling seriously ill, and some dying.
The 2017 rollout was halted; the country’s health minister, along with other officials and six Sanofi employees now await trial on charges of “reckless imprudence resulting in homicide”.
All the accused deny the charges and the company insists the vaccine is safe. But there remains an unresolved scientific mystery at the heart of the Dengvaxia tragedy: in a small subset of people, can a vaccine make an infection worse rather than better?
That question has never been more apposite. A post-coronavirus world depends on a Covid-19 vaccine. Without it, a return to normality carries the peril of more deaths from a novel respiratory virus to which humans carry no prior immunity and for which there are no life-saving treatments.
One drug authorised for treating Covid-19 patients, remdesivir, is not a game changer: it shortens recovery time but does not boost survival chances.
But a shadow looms over the global race to develop a pandemic vaccine: a little-known phenomenon called antibody-dependent enhancement (ADE), also known as disease enhancement or immune enhancement.

It refers to a counter-intuitive and potentially dangerous situation: when the presence of antibodies, which are supposed to vanquish disease, worsens rather than quells an infection.
It is a rare but not idle concern. The pandemic virus belongs to the same family of coronaviruses that causes Sars (severe acute respiratory syndrome) and Mers (Middle East respiratory syndrome). The hunt for vaccines for these 21st-century diseases — Sars appeared in 2002, Mers in 2012 — has been stymied by evidence of ADE.
Some animals that were given experimental Sars vaccines suffered more severe lung inflammation than unvaccinated animals when subsequently infected. Those trials stopped and there is still no effective Sars vaccine.
Beate Kampmann, director of the Vaccine Centre at the London School of Hygiene & Tropical Medicine (LSHTM), says that observations of ADE with previous coronaviruses mean vaccinologists must tread carefully. “We don’t want to blow the risks out of proportion but nobody can give a 100 per cent guarantee that disease enhancement won’t happen. If it does emerge here, it would be a very serious challenge.”
The emergence of ADE would be a setback for any candidate vaccine — and a cruel plot twist in the tale of Covid-19, which has turned out to be a more disruptive contagion than either Sars or Mers.
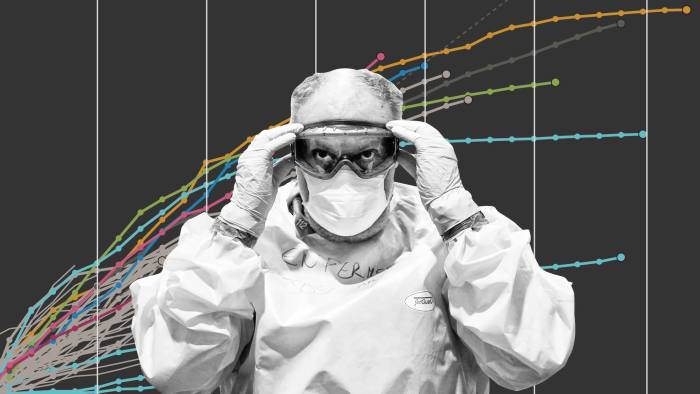
Where Sars infected about 8,000 people over eight months, Covid-19 has infected a confirmed seven million in about six months. Of those, more than 400,000 have died. The latter figures are likely to be underestimates.
The devastating health impacts go hand in hand with the biggest economic crisis since the Great Depression. Manufacturing has seen global supply chains snap; industries such as aviation, tourism, leisure and hospitality have been decimated by stay-at-home orders and social distancing; school and office closures mean missed education and precarious employment, each bringing its own long-term health consequences.
The finding that black and minority ethnic communities suffer disproportionately from the virus adds a grim social and political dimension.
A vaccine that allows people to live, work, travel, learn and socialise together safely again is the best long-term exit strategy from lockdown. This is recognised in the unprecedented number of Covid-19 vaccine projects under way: 183 by June 10, according to the LSHTM tracker.
The chances that one of those will come good seem hopeful but success is not guaranteed. There is still no vaccine against HIV, a plague that has now been with us for 40 years.
When you encounter a virus naturally, your body puts up a generalised fight to try to stop it from entering cells, which the virus needs to do to make copies of itself.
In some people, that is enough to prevent symptoms and illness. Within a week or two, a more “adaptive” response emerges: your body makes bespoke antibodies, which bind specifically to the virus, and T-cells, which remove cells that have already been infected.


Vaccines are designed to elicit this adaptive response artificially: by serving up a safe molecular doppelganger of the virus to the immune system. This masquerade tricks the immune system into generating the same antibodies and T-cells that the natural virus would.
Vaccination builds a biological “memory” of the virus but without the danger of natural infection. If the virus does come knocking, a vaccinated body should be primed and ready to fight back.
In ADE, that priming goes wrong. Instead of keeping the virus at bay, the immune system aids and abets the invader; the vaccine, which should prevent disease or make it milder, results in more severe symptoms.
When the phenomenon appeared in Sars research, vaccine development halted. But scientists cannot be sure it will always emerge during testing.
“It was only when Dengvaxia was rolled out to thousands of people that the problem of enhancement was picked up,” says Mike Turner, head of major science investments at the Wellcome Trust biomedical charity, which funds global vaccine research and played a significant role in the race for an Ebola vaccine.
The risk that an experimental coronavirus vaccine could leave a person clinically worse off is acknowledged as a “theoretical concern” in current trials.
Volunteers offering to receive Oxford University’s Jenner Institute vaccine are warned in an information sheet that their safety cannot be wholly assured.
Encouragingly, the Oxford scientists reported last month that six animals given its experimental vaccine did not suffer immune enhancement when later infected.
Humans, though, are not macaque monkeys: the real test always comes when vaccinated human volunteers encounter the virus.
Anthony Fauci, who leads the US research response to Covid-19, said as much when interviewed about another eagerly anticipated vaccine, from the US company Moderna. He spoke of the need to balance the lives saved with those that might be endangered by ADE: “So, if for every one that has enhanced illness, you save a thousand lives, I’ll take that, right?”
It is a trade-off society might be forced to consider. Pandemic vaccines are, necessarily, developed on the back of incomplete knowledge. “We have only had this virus for six months,” cautions Zania Stamataki, a senior lecturer in viral immunology at Birmingham University who is assisting the UK’s national testing effort.
“That is not enough time to evaluate if you can become infected, raise protective immunity or become reinfected again. If people can be reinfected and get worse symptoms than the first time round, that’s a telling sign that we might be dealing with disease enhancement. There is a low probability of this for Covid-19.”
The virus that causes Covid-19 is named Sars-Cov-2, for its genetic similarity to the Sars virus. It is, relatively speaking, still an immunological mystery: it is not entirely clear which parts of the immune system are triggered by the virus for some people, nor why individuals react to it so differently. Why, for example, do some healthy young people succumb while some infected centenarians survive?
When I ask Danny Altmann, a professor of immunology at Imperial College in London who co-wrote a Lancet summary on coronavirus, to rate how much we know about the immunological profile of Sars-Cov-2 on a sliding scale of zero to 10, he plumps for five.


While that still represents remarkable progress for such a new virus, he says: “It’s the missing five that matters.” Key puzzles include: which bit of the immune system delivers the killer blow to the Covid-19 virus; what is the relationship between antibodies and immunity; how long does immunity last; can someone be infected twice; what happens if there is a second wave of infection?
For example, in Covid-19, high antibody levels seem to correlate with more serious illness. Recovered coronavirus patients, in contrast, can sometimes have low or undetectable levels of antibodies in their blood.
So this is the first immunological conundrum: Covid-19 antibody levels are not a straightforward measure or guarantee of protective immunity. That is one reason why the World Health Organization questions the value of immunity certificates or passports.
Altmann agrees that “not all immunity is good immunity. Some of the really severe outcomes for Covid-19 might be due to over-exuberant immune responses. Different vaccines will stimulate different parts of the immune system and the first vaccine to get to the finishing line won’t necessarily be the best.”
This autumn could mark a turning point in the coronavirus battles: there may be positive vaccine news, and we should know whether a second wave of infection is headed our way. Last century’s Spanish flu pandemic came in three waves; the second, in the autumn of 1918, was the deadliest.
A second wave of Covid-19, which Altmann considers likely, will have two effects: those who have so far evaded the virus will be vulnerable to a first infection; and those who have recovered may be at risk of getting infected a second time. It has not yet been proven that a person can suffer Covid-19 twice; reports from South Korea suggesting instances of reinfections have been ascribed to flawed tests.
But the reinfection question is not yet settled: two milder cold-causing coronaviruses in the same family as the pandemic virus can reinfect people within a year. If reinfection is possible, then that second infection should generate antibodies — and the risk of antibody-dependent enhancement surfaces again.
Kampmann explains: “ADE is about re-encountering a virus and we don’t know what happens to re-exposed people because that situation isn’t upon us. We are in the first wave. We must carefully follow people up who have successfully beaten off Covid-19 to see if there are any nasty developments second time round. If there are, we are in a very tricky situation.”
All eyes, she says, are on Wuhan — and specifically health workers there — to see what a second wave might mean for the rest of the world. Worryingly, ADE might be implicated in a serious paediatric inflammatory syndrome that seems connected with the pandemic: many of the affected children test positive for Covid-19 antibodies.
The children whose deaths were suspected to have been connected with Dengvaxia were all naive, or seronegative, before vaccination. This means they contracted their first case of dengue, a mosquito-borne fever, after being immunised.
Dengvaxia has been withdrawn from the Philippines; in the US and Europe, it can now only be given to those with a history of prior dengue infection. There is an ongoing dispute as to whether the Sanofi trials should have picked up the risk to seronegatives before rollout.
Minimising the ADE risks of a pandemic vaccine, says Wellcome’s Mike Turner, means that trials should enrol both Covid-naive individuals and the previously infected.
Phase one trials ensure a vaccine does not cause harm; phase two, involving a few hundred people, hints at efficacy (whether vaccinated individuals are less likely to become infected than unvaccinated peers); phase three, which will number 5,000 volunteers for the Jenner Institute candidate, will reveal whether a vaccine works at scale and has any side effects.
Editor’s note
The Financial Times is making key coronavirus coverage free to read to help everyone stay informed. Find the latest here.
Turner says the vaccine development process — comprising scientific, ethical and regulatory decisions — is being concertinaed, as it was during the West Africa Ebola crisis of 2014‑16. But speed is not being traded for safety.
“A process that would normally take three to four years is being done in six weeks,” he says. “But we are not cutting corners. People are dropping routine workloads to prioritise this because it is the existential threat of the moment. If I did find people were cutting corners, I would blow the whistle. You’d get half the world refusing to take a vaccine and that’s not a risk worth taking.” Almost any vaccine, he says, is safer than having the disease.
Kampmann agrees, saying that most people she has met are ready to take a pandemic vaccine. Even she has changed her assessment of the disease, after hearing tales from the Covid-19 wards: “I initially thought, ‘The sooner I get it [Covid-19], the better.’ I don’t feel like that any more. I’m in my mid-fifties and I’m seeing people my age on ventilators. I’ll wait for the vaccine.”
Anjana Ahuja is an FT science writer
Follow @FTMag on Twitter to find out about our latest stories first. Listen to our podcast, Culture Call, where FT editors and special guests discuss life and art in the time of coronavirus. Subscribe on Apple, Spotify, or wherever you listen.




