375,000 Hoosiers to lose Medicaid coverage once COVID-19 emergency ends
An estimated 375,000 Hoosiers will lose their state-supported health coverage in the 12 months following the end of the federal public health emergency — an outcome welcomed by Indiana Gov. Eric Holcomb.
The Republican chief executive recently joined 24 fellow GOP governors in a letter urging Democratic President Joe Biden to allow his COVID-19 public health emergency declaration to finally expire in April 2023 and not be renewed again.
Alternatively, Congress could use its power of the purse to cut off pandemic-related funding even if the emergency remains in effect.
“While the virus will be with us for some time, the emergency phase of the pandemic is behind us. We have come so far since the beginning of the pandemic — we now have the tools and information necessary to help protect our communities from COVID-19,” Holcomb said.
People are also reading…
More importantly, Holcomb said ending the public health emergency once again will allow states to regularly investigate whether individuals enrolled in Medicaid health coverage continue to meet program qualifications, as well as enable states to drop those who do not.
Data presented Dec. 15 to the State Budget Committee show Indiana Medicaid rolls have swelled by nearly 800,000 lives during the pandemic to a projected April 2023 peak of 2.3 million lives, or 1 in 3 Hoosiers.
Medicaid in Indiana goes by a variety of names including the Healthy Indiana Plan, Hoosier Care Connect, Hoosier Healthwise, Medicaid Managed Care, as well as specialized programs for the disabled, institutionalized, nursing home residents, pregnant women and others.
No matter the name, each program jointly is funded by the federal government and Indiana, with the federal government generally picking up about 65% of the cost of health care for covered individuals, or 90% for Hoosiers enrolled in the Healthy Indiana Plan.
While the public health emergency remains in effect the federal government is paying an extra 6.2% of state Medicaid expenses, or about $540 million a year to Indiana, in exchange for states maintaining continuous coverage and not investigating eligibility or booting individuals who no longer qualify for Medicaid.
Holcomb said that mandate is keeping individuals on Medicaid longer than they need assistance and driving up state health care expenses, even after accounting for the extra federal funding.
“We know that a considerable number of individuals have returned to employer sponsored coverage or are receiving coverage through the individual market, and yet states still must still account and pay for their Medicaid enrollment in our non-federal share. This is costing states hundreds of millions of dollars,” Holcomb said.
Ironically, ending the public health emergency as Holcomb requests actually will further drive up Indiana Medicaid spending in the short-run because the 6.2% extra federal support will be reduced or eliminated as soon as April 1, 2023, if the public health emergency is allowed to expire or Congress cuts off funding.
Indiana Medicaid anticipates it then will take up to 12 months to identify and remove the 375,000 Hoosiers it believes no longer qualify for Medicaid, who will, in the meantime, continue using health services that cost the state more absent the extra federal share.
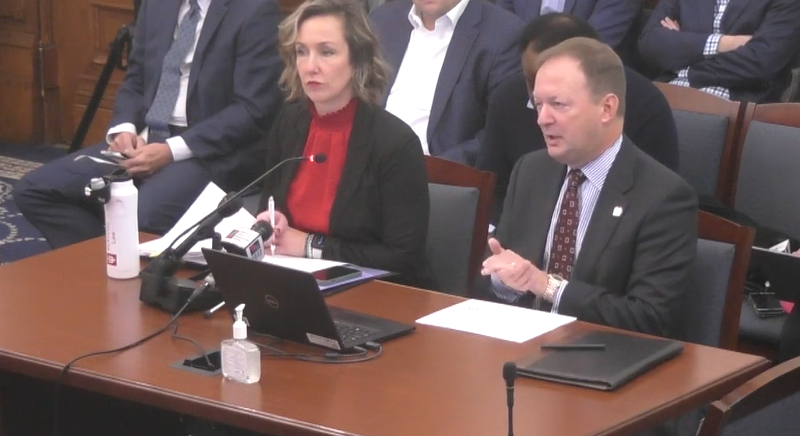
“We will start immediately looking and doing the redetermination process,” said Allison Taylor, Indiana Medicaid director. “That number (of Medicaid participants) will start to decline as soon as we hit go. But it will take 12 months to work through that volume of individuals. So we’ll see sort of an incremental step down each month.”
“Wow, man. What a scene. You can’t make up what we see out here on any given day,” Hobart patrol officer Tommie Tatum said.
Altogether, Indiana Medicaid projects the state share of Medicaid services will jump 48% to $3.5 billion during the 2024 budget year that begins July 1, 2023, and grow a comparatively normal 5.9% to $3.7 billion in 2025 — even after removing ineligible Medicaid recipients.
Most of the increased state cost is due to the loss of extra federal aid and delayed collection of the Hospital Assessment Fee and Healthy Indiana Plan contributions. But increased managed care and nursing home costs, plus 2,300 annual Medicaid-eligible births tied to the state’s near-total abortion ban also will play a role, according to Rob Damler, a Milliman actuary working for Indiana Medicaid.
The additional Medicaid expense could consume a large share of the $1.6 billion in projected state tax-revenue growth over the next 30 months, leaving little new funding available for education, public safety, quality of life grants and other Hoosier wants and needs.
Though records show Indiana should have about $900 million in unspent Medicaid appropriations from the current two-year budget that could be carried over into the next one, since the spending plan enacted in April 2021 assumed the federal public health emergency already would be over.
Here are the new Indiana laws to know that took effect July 1
Animals

The owner of a lion, tiger, leopard, snow leopard, jaguar, mountain lion or bear must prevent all direct physical contact between the animal and a member of the general public, no matter the age of the animal. Violations are subject to a $1,000 fine for each person who comes into contact with the animal. (House Enrolled Act 1248)
The owner of a lion, tiger, leopard, snow leopard, jaguar, mountain lion or bear must prevent all direct physical contact between the animal and a member of the general public, no matter the age of the animal. Violations are subject to a $1,000 fine for each person who comes into contact with the animal. (House Enrolled Act 1248)
Annexation

The Aberdeen subdivision may seek to officially become part of Valparaiso, even though the neighborhood is not currently contiguous to the city. A pre-annexation financial study must be completed so Aberdeen residents know the fiscal impact of being voluntarily annexed by Valparaiso. (House Enrolled Act 1110)
Ag equipment

Counties, cities or towns can designate agricultural zones as Economic Revitalization Areas (ERA) on the same basis as outdated business districts or distressed residential neighborhoods. New farm equipment or new agricultural improvements located in an ERA are eligible for a property tax abatement for up to five years. The exemption does not apply to farmland. (Senate Enrolled Act 119)
Bone marrow

The Indiana Department of Health is authorized to establish and promote a bone marrow donor recruitment program to find eligible Hoosiers willing to donate bone marrow to individuals fighting leukemia, lymphoma and other blood cell conditions. (Senate Enrolled Act 398)
Campus speech

State colleges and universities cannot designate outdoor areas of campus where First Amendment activities are prohibited. Higher education institutions may impose reasonable and content-neutral time, place and manner restrictions on other campus speech that’s narrowly tailored to serve a significant interest of the school. (House Enrolled Act 1190)
Caregivers

An adult relative caring for a child after the child has been removed from a dangerous home situation is entitled to directly participate in court hearings concerning services needed by the child, or terminating the parent-child relationship. Previously, only state-licensed foster parents had a statutory right to intervene in legal proceedings pertaining to abused or neglected children. (Senate Enrolled Act 410)
Catalytic converters

A catalytic converter is redefined as a “major component part” of a motor vehicle and only licensed automobile salvage recyclers are permitted to buy or sell used catalytic converters. Automobile salvage recyclers also must keep the same records for catalytic converters as valuable metal dealers and cash payouts for detached catalytic converters are capped at $25 per transaction per day. (Senate Enrolled Act 293)
Coerced abortion

A new crime of “coerced abortion” punishes anyone who knowingly or intentionally coerces a pregnant woman to have an abortion with up to 2 1/2 years in prison. State law already required “the voluntary and informed consent of the pregnant woman” prior to obtaining an abortion. (House Enrolled Act 1217)
Data breach

Businesses, banks and similar entities that suffer a data breach must notify their customers within 45 days of the breach being discovered, instead of simply providing notification “without unreasonable delay.” (House Enrolled Act 1351)
Dementia training

Home health aides who provide care to individuals with symptoms of Alzheimer’s disease, dementia or a similar cognitive disorder must complete at least six hours of dementia care training within 60 days of hire. Current home health aides with at least one year of experience must participate in at least three hours of dementia training. (Senate Enrolled Act 353)
Double voting

The penalty for fraudulently casting more than one ballot in the same election is set at up to 2½ in prison and a fine of up to $10,000. The penalty does not apply to individuals casting a valid replacement ballot as permitted by law. (Senate Enrolled Act 328)
Expungement

Individuals charged with crimes who either are acquitted following a trial or the charges are dismissed will have their court records automatically expunged within 60 days of disposition, unless the county prosecutor requests a one-year expungement delay. Any non-prosecution of criminal charges within 180 days following an arrest must be expunged immediately. (Senate Enrolled Act 182)
Foreign land purchases

Foreign business entities are barred from purchasing Indiana agricultural or timber land, with certain exceptions. Businesses organized under Russian law or controlled by Russian nationals are prohibited from acquiring any real estate in Indiana. (Senate Enrolled Act 388)
Health officers

The Indiana Department of Health no longer is entitled to remove a local health officer on the basis of intemperance. Health officers still may be removed for failing to collect vital statistics, follow rules, keep records, make reports, respond to official inquires or for neglect of official duty. (House Enrolled Act 1169)
Handguns

Adults age 18 and up legally entitled to possess a handgun are not obligated to obtain a state permit to carry a handgun in public. Indiana carry permits remain available for out-of-state reciprocity purposes. Handguns continue to be prohibited in schools, courthouses, and any residence or business that chooses to bar handguns. (House Enrolled Act 1296)
Housing shortage

A 13-member Housing Task Force is directed to study issues relating to housing and housing shortages in Indiana. The task force must submit recommendations for policy changes to the General Assembly and the governor no later than Nov. 1. (House Enrolled Act 1306)
Hunting

The holder of an archery hunting permit is allowed to use a bow and arrow or a crossbow. Previously, crossbow hunters were required to obtain a separate license. (Senate Enrolled Act 186)
Inmate calls

The in-state rate for telephone calls placed by inmates at Indiana Department of Correction facilities drops to 12 cents per minute from 24 cents per minute. County jail telephone rates are capped at 21 cents per minute statewide, instead of ranging from 22 cents per minute to $4.70 per minute. (House Enrolled Act 1181)
Lead testing

Beginning Jan. 1, 2023, doctors must offer a blood lead screening test to the parents of children between nine months and six years old if the child has not previously been tested for lead poisoning. Parents are not required to have their children tested for lead. (House Enrolled Act 1313)
Low-level felons

Judges once again may sentence level 6 felony offenders to state prisons operated by the Indiana Department of Correction, replacing a mandate that individuals found guilty of minor felony crimes only serve their six-month to 2 1/2-year sentences in county jails. (House Enrolled Act 1004)
Lowell investment

The town of Lowell is authorized to segregate its recent water utility sale proceeds from other town funds, contract with an investment adviser, and deploy the funds in most kinds of investments offering higher returns than fixed-income securities, except corporate stock and other equity securities. (House Enrolled Act 1011)
Medicaid

Pregnant individuals whose family incomes are less than 208% of the federal poverty level are entitled to receive low- or no-cost health coverage through Indiana Medicaid for the duration of their pregnancy, and up to 12 months after giving birth. (House Enrolled Act 1140)
Nuclear power

The Indiana Utility Regulatory Commission is directed to adopt rules by July 1, 2023, permitting small modular nuclear reactors to be used to generate electricity in the Hoosier State. The law does not mandate any utilities switch to nuclear power but opens the door by putting in place the regulations that would guide its development and use. (Senate Enrolled Act 271)
Pregnant inmates

Restraints used on a prison inmate in her second or third trimester of pregnancy need to be the least restrictive restraints necessary. A pregnant inmate must be unrestrained while in labor, delivering a baby and during the immediate post-delivery period, unless she is an immediate danger to herself or others, or a substantial flight risk. (House Enrolled Act 1294)
Property tax

The $3,000 property tax deduction for mortgaged property is eliminated beginning Jan. 1, 2023, and the homestead deduction is increased to $48,000 from $45,000. The senior citizen tax deduction may be claimed on homes worth up to $240,000, instead of a maximum of $200,000. (House Enrolled Act 1260)
Public comment

School boards must allow any person physically present at a school board meeting to address the board if the person is interested in doing so in accordance with the board’s public comment rules, including any time limits. Boards still can take “reasonable steps to maintain order in a meeting,” including “removal of any person who is willfully disruptive of the meeting.” (House Enrolled Act 1130)
Rape

The definition of rape is expanded to include a person who disregards the other person’s attempts to physically, verbally, or by other visible conduct refuse the person’s sexual acts. Rape in Indiana also consists of the use of force, or imminent threat of force, to compel sexual conduct; sex with a person unaware sexual conduct is occurring; or sex with a person unable to consent to sex due to mental disability. (House Enrolled Act 1079)
Semiquincentennial

A 23-member commission is established to organize events and commemorations across the state celebrating the 250th anniversary of the signing of the Declaration of Independence on July 4, 2026. (Senate Enrolled Act 12)
Simulated child porn

The production, distribution, possession or viewing of a video or image depicting obscene sexual conduct involving a person who appears to be less than 18 years old — even if the person is over 18, or doesn’t exist — is the legal equivalent of child exploitation, possession of child pornography and similar felony crimes. (House Enrolled Act 1363)
State fossil

The mastodon is designated as the official fossil of Indiana. Dozens of mastodon fossils have been found throughout Indiana, including the bones of at least five mastodons now held by the Indiana State Museum that were discovered in 2005 by workers digging a pond in the Porter County town of Hebron. (House Enrolled Act 1013)
Tax cuts

The utility receipts tax, a 1.46% charge paid by businesses and consumers on a portion of their electricity, natural gas, water, steam, sewage and telephone bills, is eliminated July 1. Beginning Jan. 1, 2023, the state income tax rate drops to 3.15% from 3.23%, with the possibility of future reductions to 2.9%. (House Enrolled Act 1002)
Tourism

The definition of “agritourism” is expanded beyond agricultural activities to include camping, canoeing, kayaking, river tubing and winter sports activities. An agritourism participant release form may be signed electronically, instead of only on paper. (Senate Enrolled Act 343)
Township trustees

A township trustee who fails to perform the duties of his or her office is subject to removal by court order if the removal is endorsed by the township board, county commissioners and county council, and other conditions are met. (Senate Enrolled Act 304)
Trans sports

All children assigned male at birth are barred from participating in any elementary, middle or high school athletics designated as a “girls” or “female” sport — no matter the child’s gender identity or physical characteristics. (House Enrolled Act 1041)
Tribal law enforcement

A police officer employed by the Pokagon Band of Potawatomi in South Bend may exercise law enforcement authority anywhere in the state, so long as the officer meets the standards of the Indiana Law Enforcement Academy and the tribe consents to statewide police powers. (Senate Enrolled Act 347)
Turn signal

A mandate that drivers signal all turns or lane changes at least 200 feet ahead of time, or 300 feet if the vehicle is traveling in excess of 50 mph, is deleted on Jan. 1, 2023, in favor of a requirement that motorists signal all turns and lane changes “a reasonable time” before completing them. (House Enrolled Act 1167)
University gifts

Public and private colleges and universities in Indiana must report to the state, and disclose on their website, all gifts from foreign entities that already must be reported to the federal government upon receipt. (Senate Enrolled Act 388)
Vaping taxes

A tax of 15% is imposed on the wholesale price of closed system cartridges used for vaping. Under a 2021 law, the tax rate was scheduled to be 25%. An additional tax of 40 cents per ounce is assessed on alternative nicotine products, such as electronic cigarettes. (Senate Enrolled Act 382)
Virtual instruction

Public schools may only hold up to three student-directed virtual instruction days during the 180-day school year absent extraordinary circumstances and a waiver approved by the Indiana Department of Education. (House Enrolled Act 1093)