A former Navy disaster specialist wages war against COVID-19 on U.S./Mexico border | Science

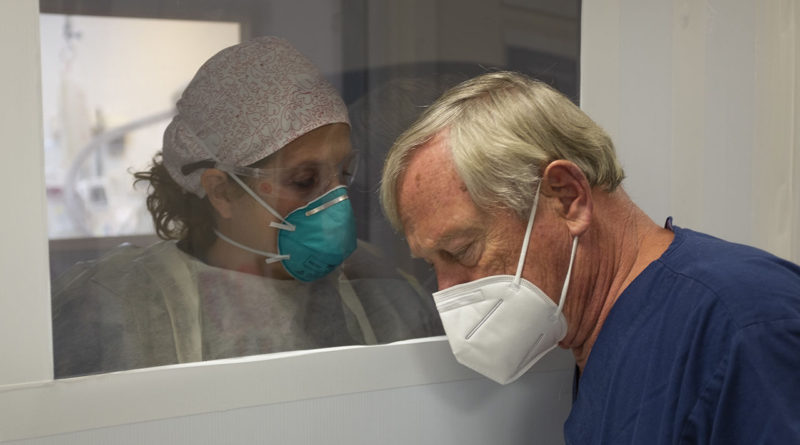
Dennis Amundson, who runs the intensive care unit at Scripps Mercy Hospital Chula Vista, chats with a nurse in the emergency room to evaluate whether a new patient might need his team’s help.
J. Cohen/Science
Science’s COVID-19 reporting is supported by the Pulitzer Center and the Heising-Simons Foundation.
SAN DIEGO—When COVID-19 patients began to pour into Scripps Mercy Hospital Chula Vista a few months ago, before the new coronavirus began to ravage much of the state, it shook up the medical team in the intensive care unit (ICU). “The morale wasn’t very good,” says Dennis Amundson, a pulmonologist who runs the ICU. They soon rallied, however, and now “smile going in” to patient rooms, he says. “It’s kind of like going to war at first,” Amundson adds. “You’re scared, and then all of a sudden you look left and look right, other people are doing it, so you do it, too. And then it becomes kind of native.”
Amundson, who 2 years ago came to this hospital a mere 16 kilometers from the border with Mexico, knows from where he speaks. During his 38-year career as a U.S. Navy clinician who specialized in disaster care, Amundson did tours in Iraq and Afghanistan, responded to tsunamis and volcanoes in Indonesia, treated Ebola patients in Liberia, and just before hanging up his captain’s hat in 2010 ran an ICU on a hospital ship off the coast of earthquake-stricken Haiti. But Amundson, who is a fit and ruddy 69 years old, says he still wasn’t fully prepared for what the pandemic has thrown at him and the hospital staff. “This certainly is a whole different animal than I was used to seeing in any of these other disasters.”
Related
Emergency room physician Juan Manuel Tovar, a 20-year veteran of the hospital who now serves as the chief operating executive, says Amundson is the perfect person to head an ICU team during a crisis. “Who is better prepared to deal with what we’re dealing with from a critical care standpoint than Denny Amundson?” asks Tovar, who still sees patients and works side by side with Amundson. “When Denny’s on and I’m on in the emergency department, I’m good. I know that no matter how hairy it gets, I got somebody who’s got my back—and that we’re battle ready.”
About half of the COVID-19 patients that Amundson’s team handles likely became infected in Mexico—most are U.S. citizens or permanent U.S. residents who live in or have recently visited Baja California. They’re seeking treatment at Scripps Mercy Hospital Chula Vista because of the shortcomings of care in Baja or because hospitals there have been overwhelmed by the pandemic. It is the busiest COVID-19 ICU in the city.
It’s early June and Amundson stands outside of one of 24 isolation rooms in the ICU that were converted to care for desperately ill COVID-19 patients. The hospital busted out an exterior window in each to accommodate large ducts, which snake up to pumps on the building’s roof that create negative pressure to suck out any aerosolized virus into high-efficiency particulate air filters. Each isolation room also has a window facing the ICU’s interior, which allows Amundson and his team to safely observe patients and only enter when necessary. Right now, he watches as five members of his team prepare to “prone” a 56-year-old, 110-kilogram, sedated man, rolling him from his back to his stomach.
The man had quickly deteriorated after he walked into the hospital 36 hours earlier, explaining that he had become ill and first sought care in nearby Tijuana, Mexico, where he was visiting his daughter. But, as Amundson’s team learned from other ICUs, when COVID-19 patients who labor to breathe are placed prone on their stomachs, their lungs readjust, frequently improving oxygen levels in a flash. “It’s almost magical,” he says.

A nurse watches a COVID-19 patient’s oxygen saturation levels rise moments after she worked with four others to “prone” the man on his belly.
J. Cohen/Science
Amundson is bare handed and has on a short-sleeved, V-neck scrub shirt and a lightweight N-95 mask. But the five-woman team of nurses and respiratory therapists in the room has donned the cumbersome full personal protective equipment: heavy-duty N95s covered by face shields, double gloves, bonnets, and gowns. “You’re in the midst of something that could harm you, maybe kill you,” Amundson says. “You have to be in there and work hard and then all of a sudden, your mask slips up a little bit, and then you fog up a little bit, and the next thing you know you’re breathing hard. There’s a little bit of pucker factor—and there’s some excitement.”
The team puts two pillows on the man’s stomach, wraps the bed sheets around him so that he looks like a corpse, and then on the count of three, quickly rotates his body without dislodging the massive ventilator apparatus jutting from his mouth. They’re in and out of the room within 15 minutes—one-third of the time it took them to prone their first COVID-19 patients. “They have their battle rhythm,” Amundson says. “Everybody has to know what they do, where they stand, and how they do it. And at first we didn’t know that. We’re learning every day.” The patient’s oxygen saturation jumps from the low 80s to 98%.
Scripps has five hospitals in its San Diego network, and the Chula Vista branch routinely transfers out COVID-19 patients, thus far preventing overload at its ICU. Today, Amundson’s ICU only has enough staff to handle 17 patients, and they’re at 15.
All these patients get “lines,” long, flexible tubing, put into their arteries and veins so that the team can easily draw blood or administer medications. Most are also on ventilators and because intubation is, in ICU lingo, “uncomfortable,” the staff sedate most of those COVID-19 patients with fentanyl and versed, an opiate/benzodiazepine combo that requires close monitoring. Taking them off the drugs has its own risks: A 38-year-old man who has been in the ICU for 1 month and is “weak as a kitten” became agitated yesterday when he regained consciousness and tried to rip out his lines, forcing them to mummy wrap his hands.
But stopping meds is a good sign. “This guy stood at the side of the bed yesterday for 8 minutes,” Amundson says. “He’s going to be a survivor.”
When patients decline and are near death, there’s a priest, chaplain, or pastor always in the ICU to offer bedside prayers and bring in, virtually, family members—who are not allowed to visit—via Zoom.
Hanna Sandor, a nurse in the unit who works three 12-hour shifts per week, says the job can wear you down. “It’s a lot,” Sandor says. “But we’re all in it together, which is the best part.”
When Science checked in with Amundson recently, he said the 56-year-old man who was gravely ill walked out of the hospital about 3 weeks after he checked in. “A save!” Amundson said. “We’re getting more out the door.” But the San Diego caseload also started to grow steadily in mid-June after the city relaxed its social distancing, one day filling 23 of his ICU’s 24 beds. “We’re in for a war,” he said, “not a battle.”