Drug design at the atomic level to thwart COVID-19
× close
Although COVID-19 has faded from the headlines, SARS-CoV-2—the coronavirus behind the pandemic—is still rampantly infecting people around the world. Public health officials fear as the virus continues to evolve, it will eventually hit upon a diabolical mutation that renders current treatments ineffective, triggering a new wave of severe infection and social disruption.
In pursuit of new therapies to avoid this dark fate, researchers at Stanford have now unveiled a compound that measures up as a potentially powerful anti-coronavirus drug, detailed in a paper published March 13 in Science Translational Medicine.
Dubbed ML2006a4, the compound works in the same way as Paxlovid—the most effective oral drug available to date—by binding to coronavirus particles and preventing the virus from making copies of itself. Compared to Paxlovid, though, ML2006a4 binds more tightly and durably, courtesy of the Stanford team custom-crafting the compound atom-by-atom.
In preclinical experiments, the compound prevented deadly infections in mice at a superior rate compared to Paxlovid. In addition, the new compound is potent enough that it could likely be formulated without an additional component present in Paxlovid that poses severe drug interaction concerns.
Importantly, ML2006a4 also performed well against coronavirus variants that have already evolved degrees of resistance to Paxlovid, suggesting the compound’s honed affinity makes it less vulnerable to mutant virus strains.
“At this point entering the fifth year of the pandemic, Paxlovid is our only really good drug against SARS-CoV-2, but it’s proven fairly easy for the virus to evolve resistance to it,” said Michael Lin, the senior author of the study, who is an associate professor of neurobiology and of bioengineering in the schools of Medicine and Engineering and a member of Stanford Bio-X.
“As new waves of coronavirus keep crashing down, we need to have alternative drugs that are more tolerant of mutations and not as easy for the virus to defeat.”
For the study, Lin worked closely with lead author Michael Westberg, now an assistant professor at Aarhus University in Denmark. From 2018 until 2022, Westberg worked in Lin’s lab as a visiting scholar at Stanford Bio-X through a joint program designed to strengthen international collaborations and the exchange of scientific expertise between Stanford and Denmark.
Atomic-level precision
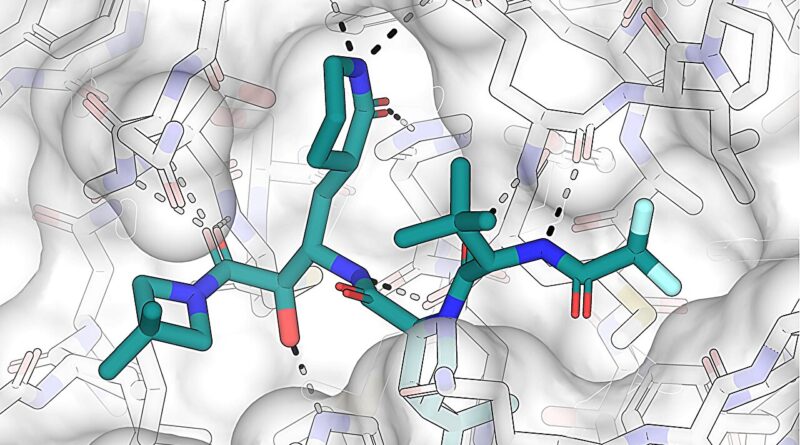
Before the pandemic outbreak in 2020, Lin’s lab had already been investigating the broad class of drugs known as viral protease inhibitors. These drugs target protease enzymes that viruses need for disassembling bulky viral proteins as part of their replication cycle. Like a key fitting into a lock, protease inhibitors occupy the spaces, or active sites, where proteases normally link up with those bulky proteins, thus nipping replication in the bud.
Specifically, the Stanford researchers had gained familiarity with hepatitis C virus protease, which has similarities to coronavirus versions. Although Westberg had come to Stanford to work on other projects, the global emergency prompted a pivot. “When the pandemic hit, we asked if we could put our expertise to good use,” said Lin.
Their early research, posted online in September 2020, demonstrated that a hepatitis C drug, boceprevir, slotted reasonably well into the coronavirus protease site. Other scientists built off those findings, including at the pharmaceutical company Pfizer, which ultimately created Paxlovid and received regulatory approval for its use in December 2021.
“We knew then that we were on the right track,” said Lin, “and we were motivated to keep going and make an even more effective drug.”
The Lin lab pooled its collective chemical knowledge to design improvements to their iterative boceprevir-based compounds. Much of the work involved modifying the compound on the atomic scale in intricately detailed computer models to fit more snugly in the coronavirus protease active site.
“Basically, you put your drug in the active site and you look for gaps where it doesn’t tightly fit. Then you fill those gaps,” said Lin.
× close
The Stanford researchers approached this challenge in a rational way by adding different configurations of atoms of carbon, nitrogen, and oxygen to the compounds as permitted by the laws of biochemistry.
“There’s a lot of creativity and intuition involved because everyone is working with the same three atoms, but there are essentially infinite ways to arrange them,” said Lin. “Making these modifications, it’s like playing atomic Tetris.”
The resulting compounds were then tested against actual coronavirus particles at the Stanford In Vitro Biosafety Level 3 Service Center. After multiple rounds of honing, Lin’s team arrived at the compound designated ML2006a4.
A promising drug candidate
In studies with SARS-CoV-2-infected mice, ML2006a4 worked as well as Paxlovid in promoting survival, while offering better protection of the rodents’ lungs and lowering overall virus load in the body.
The researchers attribute this success to ML2006a4’s extremely refined fit inside coronavirus protease, where the compound boasted a 20-fold higher binding affinity than Paxlovid. That better fit equates to stronger chemical bonds, meaning the drug can stay bound to the protease for a longer time.
In this temporal regard, ML2006a4 indeed proved quite sticky: The inhibitor remained attached for approximately 330 minutes, or greater than five hours, whereas the corresponding Paxlovid inhibitor typically fell off its target in just about two minutes.
From a medication perspective, such staying power translates to spaced-out, smaller doses that can still prevent disease from worsening while giving the immune system a chance to kill off the invaders. “The long-lived drug-enzyme complex helps ensure that the virus doesn’t escape and replicate before your next medication dose,” said Lin.
In this way, ML2006a4 offers other advantages compared to Paxlovid. Technically, Paxlovid is two drugs packaged together: nirmatrelvir, the actual protease inhibitor, and ritonavir, a drug that prevents the liver from quickly breaking down nirmatrelvir, boosting nirmatrelvir’s performance. Yet the slowing of the liver’s metabolism by ritonavir means that other drugs can toxically build up, forcing patients to take the risk of temporarily stopping their normal medications.
According to Lin, an oral pill based on ML2006a4 might not require ritonavir to prop up drug levels enough between typical 12-hour administrations to effectively keep coronavirus in check, but “this would need to be tested to make sure,” said Lin. “We also continue to make improved versions of ML2006a4 with better potency and duration of activity,” he added.
For the promising compounds to move forward, Lin and colleagues are seeking additional investment. The group now feels their compounds are ready for expanded preclinical testing with an eye toward clinical trials in human patients.
“We’re very excited how far we’ve come and how successful our drug discovery has been on a shoestring budget,” said Lin. “We hope to see this promising compound developed further to stay ready for what SARS-CoV-2 throws at us next.”
More information:
Michael Westberg et al, An orally bioavailable SARS-CoV-2 main protease inhibitor exhibits improved affinity and reduced sensitivity to mutations, Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.adi0979. www.science.org/doi/10.1126/scitranslmed.adi0979
Journal information:
Science Translational Medicine