Here’s what WHO says your mask should have to prevent COVID-19 spread

The World Health Organization on Friday updated its guidance on the use of masks amid the COVID-19 pandemic, making several changes and additions. Most notably, the agency is now recommending that governments encourage healthy members of the general public to wear masks in specific situations as part of comprehensive prevention efforts.
The new guidance puts the agency more in line with many countries worldwide that have already recommended masking the public, including the US Centers for Disease Control and Prevention which made the recommendation in early April.
However, the WHO made its updated guidance with many caveats—and some highly specific recommendations not provided by the US CDC.
“I wish to be very clear that the guidance we are publishing today is an update of what we have been saying for months: that masks should only ever be used as part of a comprehensive strategy in the fight against COVID,” WHO Director-General Tedros Adhanom Ghebreyesus (Dr. Tedros) said in a press conference Friday.
“Masks on their own will not protect you from COVID-19.”
The technical guidance, released later Friday, is equally cautious, noting “At the present time, the widespread use of masks by healthy people in the community setting is not yet supported by high quality or direct scientific evidence and there are potential benefits and harms to consider.”
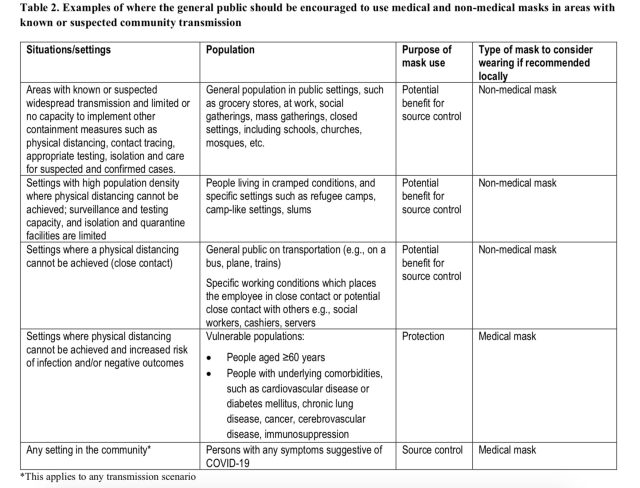
Who and when
But, the WHO’s decision to recommend masking the public was swayed by concerns that the disease spreads from infected people who don’t show symptoms (pre-symptomatic and asymptomatic transmission), according to the guidance. The agency also took into account “individual values and preferences” and the reality that physical distancing is difficult if not impossible in some contexts.
Last, the WHO emphasized that its updated guidance is based on fresh data and offers detailed technical advice on homemade mask construction.
“This is new novel research, that WHO commissioned, that we didn’t have a month ago,” Maria Van Kerkhove, WHO’s technical lead on the COVID-19 response, said in the press conference Friday.
Specifically, WHO now recommends that healthy members of the public wear homemade or commercially-available fabric masks in places where the new coronavirus is circulating widely and where physical distancing (staying 6-feet apart, etc.) is not possible or is difficult.
Detailed design
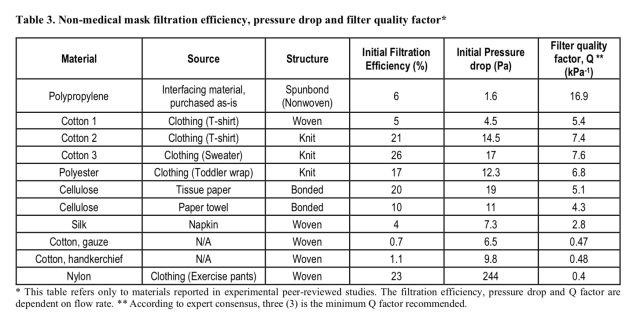
And those recommended masks aren’t just any face coverings. The agency looked over the filtration and breathability of a variety of common fabrics and materials. It noted that the French Standardization Association (AFNOR Group) has developed a technical standard for non-medical masks, which includes a minimum of 70 percent solid-particle filtration or droplet filtration.
The WHO noted that breathability—the difference in pressure across the mask as you breathe, reported in millibars (mbar) or Pascals (Pa)—should be below 49 Pa/cm2 for a medical mask. But, for non-medical masks, an acceptable pressure difference should be below 100 Pa.
Last, the WHO calculated the filter quality factor, dubbed “Q,” which is a function of filtration and breathability, with higher values indicating better overall efficiency. The bare minimum for homemade fabric mask should be Q of 3, according to WHO expert consensus.
Next, the analysis turned to assembly of the mask—the best materials and layering method. Folding a single fabric into two layers can boost filtration two to five times. Folds making four layers boosts filtration up to seven times.
The WHO determined that a minimum of three layers is required for fabric masks. But, masks may need more, depending on the fabric used. For instance, folding cotton handkerchiefs into four layers still only led to maximum filtration efficiency of 13 percent, the WHO noted. Notably, the homemade masks recommended by the US CDC only have two or three layers of cotton.
With the lower standards even for the best homemade masks, the WHO stressed that these masks are for source control only, not personal protection—that is, they can help prevent the person wearing the mask from spreading the virus, but they will not necessarily protect the wearer from becoming infected. As such, it’s important that mask wearing should always be accompanied by frequent hand washing and physical distancing.
In all, the expert analysis landed on this mask design:
The ideal combination of material for non-medical masks should include three layers as follows: 1) an innermost layer of a hydrophilic material (e.g. cotton or cotton blends); 2), an outermost layer made of hydrophobic material (e.g., polypropylene, polyester, or their blends) which may limit external contamination from penetration through to the wearer’s nose and mouth; 3) a middle hydrophobic layer of synthetic non-woven material such as polypropylene or a cotton layer which may enhance filtration or retain droplets.
Van Kerkhove noted in the press conference that “the evidence we have through this research is that, with those three layers and in that combination, that fabric [masks] can actually provide a mechanistic barrier. If someone were infected with COVID-19, it could prevent those droplets from going through and infecting someone else.”

The guidance didn’t offer specific details on the testing of the recommended mask design or comparisons with others, such as those recommended by the CDC. Ars has reached out to WHO for additional data and will update this piece if it is available.
In addition to the fabric masks for public use, the WHO is also now recommending that in areas where COVID-19 is spreading, all healthcare worker always wear medical masks—even if they are not treating COVID-19 patients specifically.
And, in areas with COVID-19 spread, all people aged 60 years or over and anyone with an underlying health condition should wear a medical mask when physical distancing is not possible.
Last, the WHO offers advice on washing your mask and how to safely put it on and take it off.
“Masks are not a replacement for physical distancing, hand hygiene, and other public health measures,” Dr. Tedros said. “Masks are only of benefit as part of a comprehensive approach in the fight against COVID-19. The cornerstone of the response in every country must be to find, isolate, test, and care for every case and to trace and quarantine every contact. That is what we know works. That is every country’s best defense against COVID-19.”




