Most sensitive COVID-19 platform runs highest volume of Hawaii tests
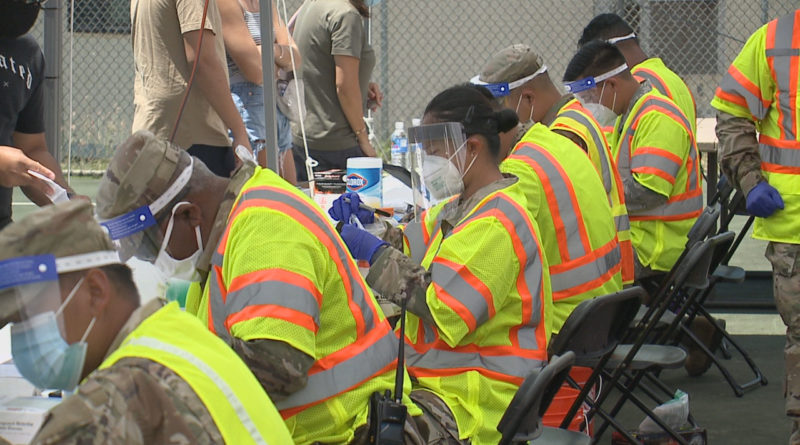
HONOLULU (KHON2) — Hawaii is testing thousands of people every day for COVID-19 to see how prevalent the virus is in our community. But are all tests created equal? Always Investigating scoured the numbers to find out.
Hawaii’s Weather Station–Visit KHON’s storm preparation page here.
One of the ways these tests vary is in how little of the virus they can detect in a sample. The most sensitive platform is churning out Hawaii’s highest volume of tests.
Always Investigating surveyed state and private labs and found about 15 different testing platforms in use. With a combined peak daily capacity of nearly 9,000, they’re averaging a collective 3,500 or so COVID-19 tests per day.
Hawaii labs ramped up testing over the summer, and positive cases spiked. Most tests were analyzed on the most sensitive platform in use in Hawaii: the Hologic Aptima SARS-CoV-2 assay.
Just last week the FDA ranked 55 authorized tests by “limit of detection” — the lowest amount of the virus the test can pick up.
“A lower LoD represents a test’s ability to detect a smaller amount of viral material in a given sample,” the FDA explained, “signaling a more sensitive test.”
Hologic’s LoD was three times lower than the Roche Molecular Systems test, also in use in Hawaii, and 30 times lower than the CDC 2019-nCoV Real-Time RT-PCR Diagnostic panel that the state lab uses.
“So what you have to think about is, how often is that really significant?” explained Dr. Edmund Desmond, the State Laboratories Division administrator. “When somebody’s really got the disease, there’s enough virus to be detected even by the less sensitive CDC method. If patients have very high levels of virus in their nasopharynx or nose when they have COVID, then the LoD is not that important and methods which have different LoDs may actually have similar sensitivities.”
Desmond explained while Hologic has the advantage of high volume, it doesn’t give key data doctors like to see for determining if someone is likely contagious, or on the downswing or upswing of the virus cycle.
“When you choose that instrument (Hologic) you have to realize that you are giving up the ability to report a CT value,” Desmond said.
CT value stands for cycle threshold which is how much a virus sample has to get amplified to be detected.
“A low CT value means that there was a lot of the virus there in the sample,” Desmond explained. “What they found in the CDC studies is that when a person is no longer infectious and no longer has infectious virus that they can culture, their CT value seems to be above 33.”
The vast majority of the state lab’s positives have been under 30 CTs. About 1 in five are under 35, and fewer than 5 percent have been just below the cutoff of 40.

They’re not too worried about misdiagnosing anything above the cutoff, which would classify negative, because the risk of missing oncoming COVID-19 is minimal. High CT traces can stick around for weeks in people long recovered from COVID-19, whereas viral loads pile on very fast when people are just getting sick.
“People who are just developing their infections and have a low viral count and a high CT value, that only lasts for a few hours,” Desmond said. “So the probability is that if you’ve got something with a high CT value it’s more likely a convalescent person than a person with a developing infection.”
The lab with the highest daily capacity is Clinical Labs of Hawaii, using the Hologic platform. Their spokesperson told KHON2: “The Hologic Aptima assay is a qualitative assay, positive or negative is decided by the instrument software so we cannot provide you with a (CT) value or ranges.”
Studies comparing platforms seem to peg the Hologic at around a 37 max CT-equivalent cutoff for a positive, when compared to samples that came up positive on other machines that yield CT numbers.
Another major lab in Hawaii, Diagnostic Laboratory Services Inc., declined to share CT data with KHON2, stating “Not all tests generate a Ct, and for those that do, it is not a reportable value according to FDA EUA labeling. At this time CT data from DLS will only be released to authorized public health officials or as part of a Queen’s Institutional Review Board approved study.”
A low CT value does not mean a person feels stronger symptoms Lt. Gov. Josh Green tells me his CT was 20 on his state lab test positive COVID, result but his worst symptom was fatigue.
“I also developed a cough over the last weekend,” Green said. “It was just basically like I had an upper respiratory infection, not that unlike having a flu. I was in the very mild symptom category.”
That’s been the experience for most of the people who got COVID during the summer spike, in which positives shifted to majority younger, generally healthier and often asymptomatic people.
Average daily positives shot up more than 1,000 percent between mid-July and late August, adding thousands of cumulative cases, but COVID hospitalizations remained in the hundreds and the ICU occupancies of COVID patients spiked below 60.
The federal Department of Health and Human Services (DHHS) has not provided CT ranges or equivalents for the Honolulu surge testing, but the FDA ranks those ThermoFisher TaqPath HealthQuest Esoterics tests, which have you swab your nostril, as about as sensitive as the state lab’s deep-sample method.
“You get a slightly higher number of positives from the nasopharyngeal, the deeply inserted swab, but the difference was slight and not statistically significant,” Desmond said. “My feeling at the moment is that the nasal swabs are good.”
At last count the DHHS’ contracted labs had processed about 58,000 Honolulu surge tests and found nearly 350 positive. That’s much a lower positivity rate than other Hawaii lab and clinic tests, but local tests have tended to be of those sick and exposed, whereas the surge tested anyone who wanted one.
“This shows that with 0.6 percent of them positive among a population of about 1 million, we’ve got 6,000 people in our population who are not diagnosed,” Desmond said, “and when you look at that number you think: ‘I want to wear a mask.’”
Just before the Honolulu surge testing got underway, the ThermoFisher TaqPath was the subject of an FDA alert about “a risk of false results.” Always Investigating followed up with the DHHS and labs responsible for running Honolulu’s tests
A DHHS spokesperson told KHON: “eTrueNorth’s laboratories using the TaqPath reached out to Thermo Fisher immediately after the announcement was made.”
HealthQuest Esoterics, an eTrueNorth subcontractor and the only labs to run Honolulu’s results, said in a statement: “During method development and validation, we identified the appropriate vortex and centrifugation parameters necessary for accurate and consistent results. Concerning the software packages Applied Biosystems COVID-19 Interpretive Software v1.2, v2.0 and v2.2 and potential false results, HealthQuest Esoterics has never implemented data interpretation with these software packages as we noticed inconsistencies early on during development. We worked with the engineers at ThermoFisher Scientific and have been utilizing the Design and Analysis Software Version 2.4.3, QuantStudio 6/7 Pro systems.”
As for other options continuing to grow in usage, Desmond describe differences between point-of-care testing versus PCR methods: “Point of care tests can be done in a doctor’s office or a nursing home or in an infirmary or a prison, they don’t have to be done in a sophisticated laboratory. Point-of-care tests are less sensitive, so if you’ve got somebody who is recovering from viral infection and they’re shedding just fragments of virus, real-time PCR laboratory tests which are more sensitive will still be positive and these point-of-care tests will become negative.”
Desmond says the separate category of tests known as antigen tests, already less sensitive than the genetic PCR methods, are proving questionable.
“We’re maybe willing to accept that because the people who are negative by antigen maybe are not infectious. But there have been reports of false positive results with this,” Desmond said. “I think there really has to be a responsibility taken by the manufacturer of these antigen tests to do a root cause analysis and find out when there are false positives what caused this. They have to behave responsibly.”