Putting low-cost diagnostics to the test

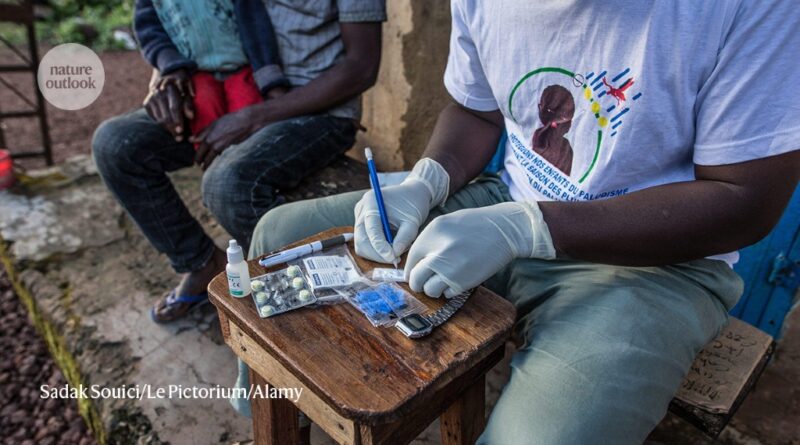
Rapid diagnostic tests for malaria have an important role in areas with limited access to health care.Credit: Sadak Souici/Le Pictorium/Alamy
Nobody enjoys twirling a swab up their nose to test for COVID-19, but many people had cause to be grateful for at-home diagnostic tests during the height of the pandemic. Users could learn in 15 minutes whether they were infected with the coronavirus and were at risk of exposing friends or family to COVID-19 — all without leaving the house.

Part of Nature Outlook: Medical diagnostics
These rapid antigen tests are much less accurate than laboratory-based diagnostics. But in many countries, they filled crucial gaps in otherwise overextended health-care systems, directing mildly ill or asymptomatic people away from unnecessary medical care. “During the pandemic, I had to give so many webinars, and talk with so many governments about how we were not trying to push the rapid antigen test as a second-best tool to use,” says Rosanna Peeling, chair of diagnostics research at the London School of Hygiene & Tropical Medicine.
Unfortunately, many people in low- and middle-income countries (LMICs) found themselves hard pressed to obtain any kind of testing — either home or lab based. And this problem existed long before COVID-19. “We were actually living with a pandemic already,” says Tivani Mashamba-Thompson, a diagnostics specialist at the University of Pretoria in South Africa. “We were living with the HIV pandemic, with a tuberculosis pandemic — these needed the same systems, but nothing was ready.” And unlike in wealthier nations, simple point-of-care diagnostic tests in LMICs are not merely a stopgap — they might be the only option, given the limited access to well-equipped clinics and hospitals. Indeed, Mashamba-Thompson says that she grew up in a village in rural Limpopo that to this day has no clinic.
If the technologies mobilized against COVID-19 could be broadly applied to low-cost point-of-care diagnostics for other conditions, this dearth of testing could become an unhappy memory, and biomedical engineer Jonathan Cooper at the University of Glasgow, UK, sees a clear opportunity. “The pandemic showed that you can make tests relatively quickly and get through regulatory pathways relatively successfully,” he says. But turning a laboratory concept into a real-world public-health success remains exceedingly difficult, particularly for people in the world’s most resource-limited regions.
Seeking reassurance
In 2004, Peeling and her colleagues coined the acronym ASSURED to describe key considerations for rapid diagnostic tests for sexually transmitted infections (STIs) for use in LMICs1. The researchers stipulated that tests should be affordable, sensitive, specific, user-friendly, rapid, equipment-free and deliverable to the communities that need them. These criteria were quickly applied to point-of-care diagnostic assays in general. Around a decade later, they were renamed REASSURED to accommodate two more priorities: real-time reporting capabilities and easy sample collection2.
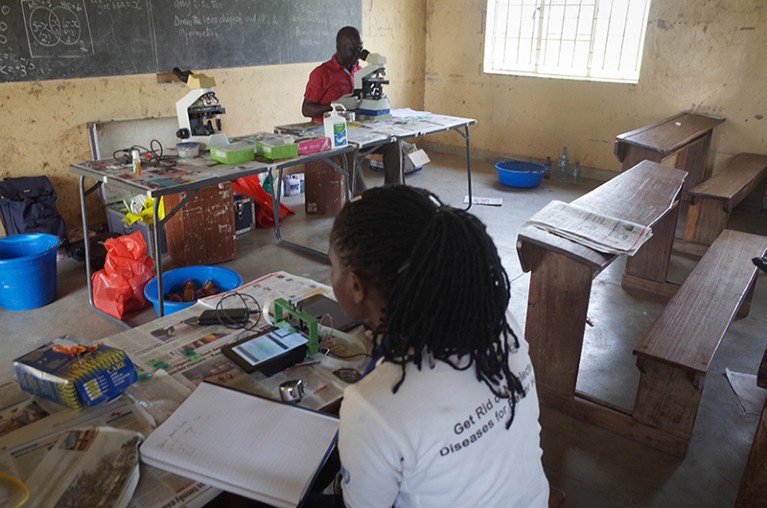
Researchers test how their rapid isothermal amplification malaria tests could be used in a school in rural Uganda.Credit: Jonathan Cooper
Although these acronyms provide a helpful point of reference when developing tests, it is unlikely that any one technology will tick all the boxes. Trade-offs are inevitable, and appropriate thresholds for an assay’s performance in one domain will depend on how well it scores in another. For example, diagnostics that offer only modest sensitivity — such as at-home COVID-19 tests — can still deliver a massive public-health win if they greatly expand the population who will be directed to the appropriate follow-up care. “We still have regions of the world where there’s no diagnostic testing available at all,” says Cooper.
A few effective low-cost diagnostics are already in widespread use, including rapid tests for malaria that cost just over US$2 per assay. But many commercially available rapid diagnostic systems — even those that have made a difference in LMICs — fall short of the REASSURED criteria.
For example, Peeling says that the GeneXpert platform for detecting viral and bacterial DNA and RNA has “revolutionized the diagnosis of tuberculosis” in resource-limited settings. However, this system, developed by Cepheid in Sunnyvale, California, is generally used in formal medical centres and requires a costly — upwards of $15,000 — instrument, which is bulky and requires steady access to power. “They aren’t really suited for somebody with a backpack going into a small village,” says Paul Yager, a biomedical engineer at the University of Washington in Seattle. A test developed by Visby Medical of San Jose, California, for STIs and respiratory infections takes instrumentation out of the equation. The standalone test can be read directly by the user, but carries a screening cost of roughly $80 per test.
Finding the fast track
A new generation of assays under development could reduce testing costs without sacrificing too many other criteria. Bhushan Toley, a chemical engineer at the Indian Institute of Science in Bengaluru, says that his country’s government is pushing for tuberculosis tests that cost under $4. “It’s really tough to meet those price points,” he says, adding that the margins can be narrower in especially low-income regions. “A dollar test seems very cheap in the United States, but it may or may not be elsewhere.”
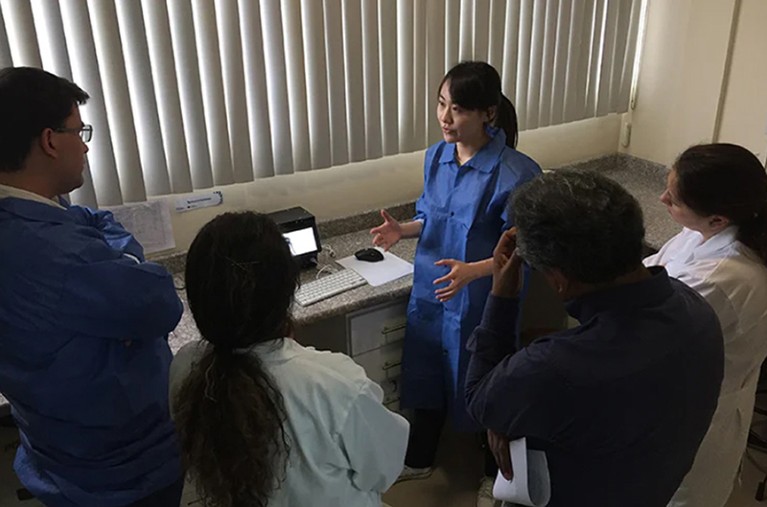
A researcher explains how to use isothermal DNA amplification testing equipment for Zika and chikungunya viruses in Ecuador as part of trials in Latin America.Credit: Pardee Lab., Univ. Toronto
As an alternative to standard lab materials such as glass and plastics, many groups are cutting costs by performing tests on paper, which naturally absorbs fluids and can be precisely shaped and patterned with channels, reagents and other elements using tools such as ink-jet printing. Indeed, paper-based assays are already commonplace for pregnancy tests and at-home COVID-19 diagnostics. In parallel, Yager points to advances in protein engineering and formulation that are making it increasingly straightforward to store enzymes and other crucial reagents in a stable, dried form that can quickly recover normal function when rehydrated. This can eliminate the need for refrigeration, simplifying shipping and storage at off-the-grid locations.
Most at-home COVID-19 tests are lateral flow antigen-detection assays, in which fluid from a sample is added to a reservoir containing dye-labelled antibodies against the spike protein of the virus SARS-CoV-2. If that protein is present, it binds to these antibodies and flows along the paper through capillary action until it reaches the detection zone: another strip of antibodies that captures the labelled viral protein and produces a distinctive coloured stripe as a readout. Such tests are a mainstay of modern diagnostics. But antigen tests can also be difficult to update, requiring considerable effort to develop new antibodies if a pathogen changes. Cooper cites the example of malaria: evolution of the causative parasite Plasmodium falciparum — specifically, the discarding of hrp2 and hrp3 genes — enables it to elude diagnosis by rapid diagnostic tests that target the antigens encoded by those genes.
Nucleic-acid-based tests are easier to adapt to evolving targets than are antigen tests, and can be much more sensitive. Most lab tests use a process called the polymerase chain reaction (PCR) to rapidly amplify tiny quantities of pathogen DNA or RNA to detectable levels. However, PCR is tough to do on the cheap, because it requires specialized equipment that can cycle the sample through a range of temperatures with high precision. A powerful alternative is a process known as isothermal amplification, which can be carried out at a single fixed temperature. Cooper’s team developed a paper-based test that uses such a reaction. The test was 98% accurate in detecting malaria during a field test in Uganda, overcoming the blind spot of current antigen tests as a result of missing hrp genes3. However, isothermal amplification tests still require access to a stable heat source.
REASSURED calls for equipment-free testing both to cut costs and because electricity is not reliably available in many parts of the world. But a dedicated sample-preparation or assay-reading instrument need not be a dealbreaker if it is designed with the limitations of the setting in mind. Mashamba-Thompson notes that even wealthy South African communities routinely deal with rolling blackouts, and that “you can go to places in Mozambique and Zimbabwe where the electricity is not there”. But simple battery-powered systems are an acceptable alternative, and many emerging point-of-care diagnostic tests exploit smartphones, which are accessible in many otherwise resource-limited settings. The role of phones can range from mere sources of electrical power to a way to analyse assay results or upload those results to public-health databases. Indeed, the test devised by Cooper and his colleagues exploited these capabilities.
But phones also pose challenges, including variable performance of sensors and cameras from different makes and models — or even from the same model in different lighting conditions. This can confound efforts to use smartphone cameras as a reliable tool for assay interpretation. And Peeling says that the US Food and Drug Administration, which often sets the pace for global medical-device regulations, has been hesitant to approve phone-based diagnostics because of the frequency with which the software of phones changes. “Maybe after the pandemic, we can seriously talk about phones as a medical device,” she says. “But right now, no.”
Reality check
An engineer’s best-laid plans can quickly fall apart when the time comes to test an assay in a clinical setting. Many designs never leave the laboratory, and there are only a handful of successful field trials in the scientific literature. Nevertheless, some promising results are trickling in. For example, last year, a team led by Keith Pardee, a synthetic biologist at the University of Toronto, Canada, reported the results of a trial he conducted in three Latin American countries for a paper-based assay that uses isothermal DNA amplification to detect Zika and chikungunya viruses in human serum. The assay achieved nearly 99% accuracy in detecting both viruses4.
Researchers from an international team led by specialists at the University of Toronto test a portable diagnostic technology in Brazil.Credit: Pardee Lab., Univ. Toronto
Even in the controlled and supervised conditions of a field trial, unexpected setbacks are commonplace. “There was so, so much failure,” says Pardee. “It’s really hard to pick up shop and move to a place that’s not your lab.” One challenge that can emerge when sample collection and handling are no longer being carried out by seasoned lab staff in an environmentally controlled setting is contamination. Cooper recalls a field trial of his team’s paper-based malaria diagnostic test at schools in Uganda that was routinely undone by stray DNA infiltrating the assay materials. “On day one, everything works 100% of the time,” says Cooper. “By day three, even your distilled water is testing positive.”
Field-trial veterans highlight the importance of engaging early with regional partners who can give a much-needed reality check during assay development. This means becoming intimately acquainted with the limitations of the infrastructure of the sites where testing will happen and the way that diagnostic tests are used in health-care systems. These considerations are central to Mashamba-Thompson’s research. She says that the public-health returns from diagnostics efforts in LMICs are frequently undermined by failure to recognize the needs of patients, the skills and capabilities of the people applying the test, or the organizational structure of local health-care systems. In some cases, for example, tests in resource-limited settings might be carried out by people with limited literacy skills. And even in reasonably well-equipped clinics, health-care workers might not be trained in how to handle the diagnostic process as part of their workflow. During the pandemic, Mashamba-Thompson says, “nurses were not happy about now having to do the work that is usually done by laboratory professionals”.
Cooper hopes to overcome these hurdles with the DIDIDA (Digital Innovations and Diagnostics for Infectious Diseases in Africa) project, which is bringing together European and African scientists and health-care specialists as well as government officials and educational institutions to develop, test and deploy low-cost, smartphone-coupled diagnostics in sub-Saharan Africa for diseases such as typhoid, tuberculosis and malaria. “There are three pillars to the project — detecting diseases, and then collecting the data, but also capacity strengthening,” explains Cooper.
Accessibility of reagents has been an especially difficult hurdle for test deployment in LMICs. Toley’s team develops paper-based nucleic-acid detection assays, and he says that it still relies heavily on Western sources for costly reagents such as enzymes — and even the high-quality paper materials used in tests can be difficult to source in India. To address this, the country has launched the Indigenization of Diagnostics network as a means to broaden access to crucial materials and reagents. “They are trying to get a lot of local innovators together to help each other out,” says Toley. And in Africa, the DIDIDA project is working to strengthen local capacity through training and education, while also facilitating regional manufacturing of diagnostic tests at sites such as the Pasteur Institute of Dakar in Senegal.
As an added benefit, local manufacturing capacity can also fuel development of diagnostics for conditions that are endemic in LMICs, but of minimal concern to wealthy nations — or biotechnology companies. “Chikungunya, for instance, is not a priority for large parts of the industrialized world,” says Pardee. “There’s huge potential in having the capacity to make tests that are relevant in those markets.”
More generally, the point-of-care diagnostics approaches that are essential to affordable detection of diseases in LMICs have long been neglected. The sense of urgency brought on by the COVID-19 pandemic — particularly before the arrival of vaccines — has already begun to fade, but Mashamba-Thompson hopes that the world has not forgotten entirely the lessons of this experience. “It was clear that the first point of contact with the health-care system during the pandemic was through diagnostics, and it still is,” she says. “And it’s important to just keep that momentum to ensure that when the next pandemic hits us, we don’t have to start from scratch again.”