Should we ration extracorporeal membrane oxygenation during the COVID-19 pandemic?
Experts have recommended that ECMO be curtailed or even halted when patient numbers surpass an ill defined threshold, wherein demand for critical care outstrips available resources.
It might seem counterintuitive to reduce the provision of ECMO at precisely the time when demand increases, yet it could be deemed necessary. In this Comment, we argue that a decision to curtail or continue ECMO should be deliberate and reasoned, such that alternatives are actively rejected.
Both modalities are complex and can entail a prolonged ICU stay; however, the resource intensity of ECMO is typically higher, especially with respect to ICU staffing.
Therefore, if ICU staff are the primary scarce resource, cessation of an ECMO programme might result in more patients being treated. However, if it is not staff that are scarce, but mechanical ventilators or ICU beds, the same might not hold true.
The value of ECMO is not universally accepted as part of established critical care in the way that mechanical ventilation is; therefore, access to ECMO might not be regarded as a right equal to access to mechanical ventilation.
- Hick JL
- Christian MD
- Sprung CL
It is particularly challenging to identify the specific point in time during a pandemic when crisis standards of care should be adopted. Unlike a single mass casualty event, the experience with COVID-19 suggests that the process will be dynamic during a pandemic, with a threshold that is crossed more than once in both directions, and that different resources will be constrained at different points in time.
Furthermore, it has been clear that many governmental agencies will be reluctant to invoke crisis standards of care for political reasons, even when potentially lifesaving treatments, which under normal conditions are available in sufficient quantities to everyone who needs them, become scarce and must be rationed at individual hospitals to a much greater degree than under normal circumstances.

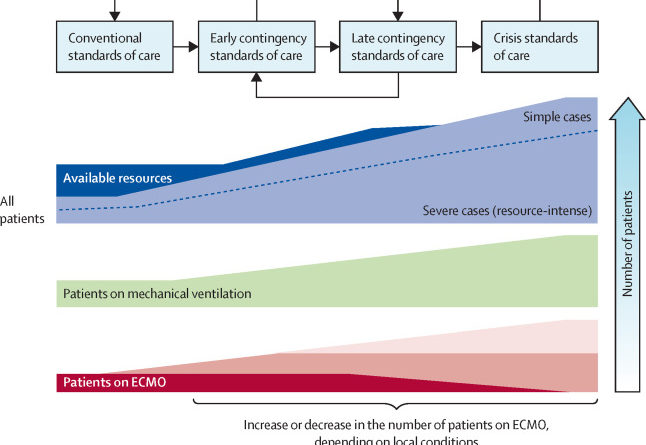
FigureTransitioning between standards of care during an acute crisis
Before life-saving treatments are rationed, efforts should be taken to extend available resources and to use them most efficiently and effectively. These efforts have to be continued, even after entering crisis standards of care, to return to a previous step as soon as possible. Depending on the ethical principles adopted and patient characteristics, levels of ECMO offered could be the same as those provided during normal circumstances, reduced, or even increased during the transition from normal to crisis standards of care. ECMO=extracorporeal membrane oxygenation.
,
Ideally, this prioritisation exercise should occur before a crisis occurs. However, during the COVID-19 pandemic, such consensus had not been achieved in time to act. In this situation, experts, professional organisations, and governments must attempt to reach agreement on the principles to be applied to guide bedside clinicians who have no choice but to make such decisions, with or without the guidance of society at large.
Before assuming that rationing of ECMO is the optimal approach, the validity of the argument and the underlying principles should be disclosed and discussed, and the alternatives explicitly rejected.
Limited resources should then be distributed in a way that allows health systems to achieve the highest number of lives saved. This approach could result in reduced, unchanged, or even increased numbers of patients being treated with ECMO, depending on the specific resources in scarcity and the purported effectiveness of ECMO use in the patients in question. If an approach more focused on individual rights is favoured instead, emphasis will be on guaranteeing a fair process for the distribution of scarce resources. Again, although this choice might result in reducing the number of patients treated with ECMO, there are circumstances in which this will not be the case.
Under crisis standards of care, with an overwhelming number of patients competing for a scarce resource (eg, mechanical ventilation or ECMO), a thorough comparative assessment of individual risks and prognosis will be challenging. Therefore, final allocation decisions and commitment to the degree to which ECMO services can be provided require careful assessment of the specific resources that are scarce, the (additional) resources required for ECMO at a given centre, and the effect on other patients of choosing to offer ECMO to a specific patient in this environment. Further changes in ECMO technology, the human resources needed, or the evidence base supporting ECMO could alter the balance of whether or not to provide ECMO during late contingency or crisis standards of care during a pandemic.
If a centre has had no survivors among their patients treated with ECMO during a crisis, this should be factored into decision making. However, if many patients are believed to have survived because of ECMO, this should prompt greater consideration of the intervention, even in the context of waning resource availability.
There is neither an ethical nor an operational imperative requiring the cessation of ECMO services during a public health crisis, such as the COVID-19 pandemic. Ethical principles and triage guidelines based on these principles might or might not result in the cessation of ECMO services when demand outstrips available resources, depending on the circumstances and the choices made. Importantly, we believe that cessation of ECMO is an ethical option that should be explicitly considered during late contingency and crisis standards of care.
AS reports research grants and lecture fees from CytoSorbents and lecture fees from Abiomed, outside of the submitted work. DB reports grants from ALung Technologies; personal fees from Baxter, Xenios, and Abiomed; and unpaid consultancy for Hemovent, outside of the submitted work. JRC reports grants from the National Institutes of Health and the National Palliative Care Research Center, and grants and personal fees from Cambia Health Foundation, outside of the submitted work. All other authors declare no competing interests.
Supplementary Material
References
- 1.
Fair allocation of scarce medical resources in the time of COVID-19.
N Engl J Med. 2020; 382: 2049-2055
- 2.
ECMO during the COVID-19 pandemic: when is it unjustified?.
Crit Care. 2020; 24: 507
- 3.
Case characteristics, resource use, and outcomes of 10 021 patients with COVID-19 admitted to 920 German hospitals: an observational study.
Lancet Respir Med. 2020; 8: 853-862
- 4.
Randomised controlled trial and parallel economic evaluation of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR).
Health Technol Assess. 2010; 14: 1-46
- 5.
ECMO for ARDS: from salvage to standard of care?.
Lancet Respir Med. 2019; 7: 108-110
- 6.
European Society of Intensive Care Medicine’s Task Force for intensive care unit triage during an influenza epidemic or mass disaster. Chapter 2. Surge capacity and infrastructure considerations for mass critical care. Recommendations and standard operating procedures for intensive care unit and hospital preparations for an influenza epidemic or mass disaster.
Intensive Care Med. 2010; 36: S11-S20
- 7.
Allocating scarce intensive care resources during the COVID-19 pandemic: practical challenges to theoretical frameworks.
Lancet Respir Med. 2021; 9: 430-434
- 8.
COVID in NYC: What New York did, and should have done.
Am J Bioeth. 2020; 20: 153-155
- 9.
Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal.
BMJ. 2020; 369m1328
- 10.
Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic.
JAMA Intern Med. 2020; ()
Article Info
Publication History
Identification
Copyright
© 2021 Elsevier Ltd. All rights reserved.
ScienceDirect
Linked Articles
- Allocating scarce intensive care resources during the COVID-19 pandemic: practical challenges to theoretical frameworks
-
The COVID-19 pandemic strained health-care systems throughout the world. For some, available medical resources could not meet the increased demand and rationing was ultimately required. Hospitals and governments often sought to establish triage committees to assist with allocation decisions. However, for institutions operating under crisis standards of care (during times when standards of care must be substantially lowered in the setting of crisis), relying on these committees for rationing decisions was impractical—circumstances were changing too rapidly, occurring in too many diverse locations within hospitals, and the available information for decision making was notably scarce.
Full-Text
PDF
-