Successful Elimination of Covid-19 Transmission in New Zealand
To rapidly communicate short reports of innovative responses to Covid-19 around the world, along with a range of current thinking on policy and strategy relevant to the pandemic, the Journal has initiated the Covid-19 Notes series.
Soon after initial descriptions of an outbreak in Wuhan, China, were shared, reports in late January 2020 (https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30260-9/fulltext) confirmed that Covid-19 was almost certain to become a serious pandemic. Despite New Zealand’s geographic isolation, we knew that introduction of SARS-CoV-2 was imminent because of the large numbers of tourists and students who arrive in the country each summer, predominantly from Europe and mainland China. Our disease models indicated that we could expect the pandemic to spread widely, overwhelm our health care system, and disproportionately burden indigenous Maori and Pacific peoples. New Zealand began implementing its pandemic influenza plan in earnest in February, which included preparing hospitals for an influx of patients. We also began instituting border-control policies to delay the pandemic’s arrival.
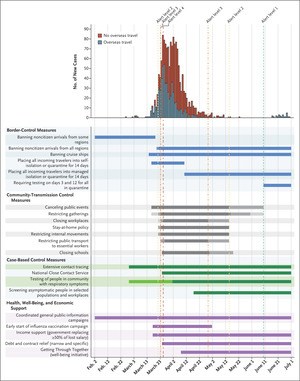
 New Covid-19 Cases in New Zealand and Implementation of Epidemic-Response and Support Measures.
New Covid-19 Cases in New Zealand and Implementation of Epidemic-Response and Support Measures.
Shown are daily new cases of Covid-19, including confirmed and probable cases, according to overseas travel status and in relation to implementation of epidemic-response measures as well as health, well-being, and economic-support measures. Darker shading represents strengthened controls or heightened measures.
New Zealand’s first Covid-19 case was diagnosed on February 26 (see Figure 1). That same week, the WHO–China Joint Mission’s report on Covid-19 (www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf) showed that SARS-CoV-2 was behaving more like severe acute respiratory syndrome (SARS) than like influenza, which suggested that containment was possible.
By mid-March, it was clear that community transmission was occurring in New Zealand and that the country didn’t have sufficient testing and contact-tracing capacity to contain the virus. Informed by strong, science-based advocacy, national leaders decisively switched from a mitigation strategy to an elimination strategy (www.nzma.org.nz/journal-articles/new-zealands-elimination-strategy-for-the-covid-19-pandemic-and-what-is-required-to-make-it-work). The government implemented a stringent countrywide lockdown (designated Alert Level 4) on March 26. During this period of exponentially increasing local cases, many people wondered whether these intensive controls would work. After 5 weeks, and with the number of new cases declining rapidly, New Zealand moved to Alert Level 3 for an additional 2 weeks, resulting in a total of 7 weeks of what was essentially a national stay-at-home order.
In early May, the last known Covid-19 case was identified in the community and the person was placed in isolation, which marked the end of identified community spread. On June 8, the government announced a move to Alert Level 1, thereby effectively declaring the pandemic over in New Zealand, 103 days after the first identified case.
New Zealand is now in the postelimination stage, which comes with its own uncertainties. The only cases identified in the country are among international travelers, all of whom are kept in government-managed quarantine or isolation for 14 days after arrival so they don’t compromise the country’s elimination status. Of course, New Zealand remains vulnerable to future outbreaks arising from failures of border-control and quarantine or isolation policies. Most jurisdictions pursuing containment (including mainland China, Hong Kong, Singapore, South Korea, and Australia) have experienced such setbacks and have responded with rapid reescalation of control measures. New Zealand needs to plan to respond to resurgences with a range of control measures, including mass masking, which hasn’t been part of our response to date.
New Zealand’s total case count (1569) and deaths (22) have remained low, and its Covid-related mortality (4 per 1 million) is the lowest among the 37 Organization for Economic Cooperation and Development countries. Public life has returned to near normal. Many parts of the domestic economy are now operating at pre-Covid levels. Planning is under way for cautious relaxing of some border-control policies that may permit quarantine-free travel from jurisdictions that have eliminated Covid-19 or that never had cases (e.g., some Pacific Islands).
The lockdown and consequent deferral of routine health care have undoubtedly had negative health effects, although total national weekly deaths declined during the lockdown (https://blogs.otago.ac.nz/pubhealthexpert/2020/07/10/weekly-deaths-declined-in-nzs-lockdown-but-we-still-dont-know-exactly-why/). To mitigate adverse economic effects, the government instituted a spending program to support businesses and supplement the incomes of employees who lost their jobs or whose jobs were threatened.
There are several lessons from New Zealand’s pandemic response. Rapid, science-based risk assessment linked to early, decisive government action was critical. Implementing interventions at various levels (border-control measures, community-transmission control measures, and case-based control measures) was effective. Prime Minister Jacinda Ardern provided empathic leadership and effectively communicated key messages to the public — framing combating the pandemic as the work of a unified “team of 5 million” — which resulted in high public confidence and adherence to a suite of relatively burdensome pandemic-control measures. Future lessons for New Zealand include the need for stronger public health agencies that can better assess and manage potential threats and for greater support for international health organizations, notably the World Health Organization.
Michael G. Baker, M.B., Ch.B.
Nick Wilson, M.B., Ch.B., M.P.H.
University of Otago, Wellington, New Zealand
Andrew Anglemyer, Ph.D., M.P.H.
University of Otago, Dunedin, New Zealand
Disclosure forms provided by the authors are available with the full text of this note at NEJM.org.
This article was published on August 7, 2020, at NEJM.org.
We thank colleagues at the University of Otago for helpful comments on this note, and we thank the Ministry of Health, the All-of-Government Response Group, our elected leaders, and the “team of 5 million” for leading and supporting the Covid-19 response in Aotearoa New Zealand. We acknowledge funding support from the Health Research Council of NZ (20/1066).