Tracking patients’ COVID-19 vaccinations likely to challenge providers
COVID-19 and the hope for a solution—a vaccine—have shined a light on yet another long-standing problem in healthcare that is likely to get worse: patient identification.
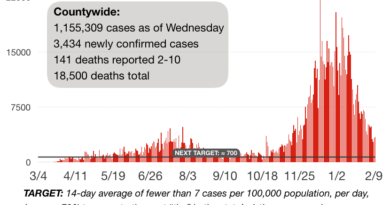
The coronavirus crisis, responsible for more than 200,000 deaths in the U.S., has brought renewed focus on patient matching, a subtle but still crucial patient safety and operational challenge hospitals have been grappling with for decades.
Without a way to accurately identify patient immunization records across care settings, providers won’t be able to track who has received a COVID vaccine—a priority for returning to a so-called new normal.
Effectively distributing and administering a vaccine requires knowledge of who has received it and who hasn’t, said Ben Moscovitch, project director for health information technology at the Pew Charitable Trusts. The process, which largely relies on providers looking up patient records in state immunization registries, “is a patient-matching issue,” he said.
Patient matching, or matching patients with their medical records, sounds like a simple concept. But while organizations have made strides in accurately matching patients to records within their own system, it’s challenging to link records with outside organizations, making it difficult for providers to get a comprehensive view of a patient’s medical history. That’s particularly true for immunizations, which can be doled out at hospitals, clinics and pharmacies across a patient’s life—and thus held in numerous systems.
The yet-to-arrive COVID vaccine puts a spotlight on those challenges, as long-standing problems will be compounded by the expected volume of patient demand and its likely status as a multidose vaccine.
“It’s the same story,” said Julie Pursley, director of health information thought leadership at the American Health Information Management Association, “just on a larger scale.”
And the COVID vaccine isn’t the only immunization challenge facing providers during the pandemic. Providers will also have to stay attuned to immunizations for the thousands of patients who delayed routine care in the spring, forgoing childhood immunizations and adult booster shots.
The Trump administration this month unveiled a national COVID vaccine distribution strategy, which includes an emphasis on using IT systems to “identify when a person needs a potential second dose, to monitor outcomes and adverse events, and to account for products the U.S. government is spending billions of dollars to research, develop, and produce,” according to a strategy report from HHS’ Operation Warp Speed. Immunization registries will be “central to this IT infrastructure,” the report reads, with Operation Warp Speed creating new IT tools to fill existing gaps.
Under the administration’s strategy, COVID vaccination data that would typically be documented in immunization registries, providers’ electronic health records and pharmacies’ dispensing record systems will be subsequently reported into a “common IT infrastructure” developed by HHS.
HHS and the Centers for Disease Control and Prevention did not return a request for comment on the system.
A ‘hodgepodge’
Immunizations are just one part of a patient’s medical history. But tracking vaccinations—from childhood into adulthood—comes with its own set of unique challenges.
Already, it’s pretty common for patients to be unsure of their own immunization history, said Dr. Corey Lyon, a family physician at UCHealth’s A.F. Williams Family Medicine Clinic in Denver. There’s a slew of vaccinations that patients are expected to receive, some of which take place during childhood with boosters every five or even 10 years in adulthood.
“A lot of times the patient will say, ‘I think so,’ or ‘I don’t know’ ” when asked about a vaccine, Lyon said. “It’s a pretty common exercise we have in trying to validate and see when patients are potentially due for an immunization.”
That problem could intensify in the wake of COVID, as fewer children received vaccinations when families delayed non-emergency care in the spring. In mid-April, at the height of the COVID pandemic, childhood vaccinations dropped by roughly 60% compared with the year prior, according to an analysis of claims data from the Health Care Cost Institute. Measles vaccinations dropped roughly 73% in April and were down 37% at the end of June, suggesting families aren’t rushing to reschedule deferred care.
It’s a trend that could have long-term effects on patients, if providers aren’t able to flag who hasn’t received expected vaccinations and offer them at future appointments.
Generally, if a patient has received all their immunizations at one organization, it’s pretty seamless to look up their history in the EHR, experts say. It gets more complicated if the patient is new to the practice or has received vaccines at other locations. Then a clinic will have to request their records from a previous provider or, if the patient’s previous provider is in the same state, can check with the state’s immunization registry.
It’s “kind of a hodgepodge,” said Dr. Lane Tassin, Western region chief medical officer at FastMed Urgent Care, a company that operates urgent-care and family medicine clinics in Arizona, North Carolina and Texas. “There’s no distinct, definite way to know if any one particular individual has received any one particular vaccination.”
Not all patients and providers participate in registries, so they’re not “an absolute guarantee,” Tassin said. States vary in making reporting to immunization registries voluntary or mandatory, as well as what particular vaccines providers are required to report.
Immunization registries, also called immunization information systems, are typically managed by state public health departments as a way to gather and consolidate patients’ vaccination data across organizations. Providers in the state can log into the registry to search for and input a patient’s immunizations, providing a record of patient vaccinations over time.
“Whether you get your hep B (vaccine) as an infant or whether you get your shingles shot at the pharmacy when you turn 50, all of those would be tracked in an immunization information system,” said Mary Beth Kurilo, senior director of health informatics at the American Immunization Registry Association.