What can cool San Diego County’s COVID-19 hot spots?
For the past three months, the novel coronavirus has hit the people living in a handful of San Diego County ZIP codes the hardest, a trend that has generated increasingly forceful cries for help.
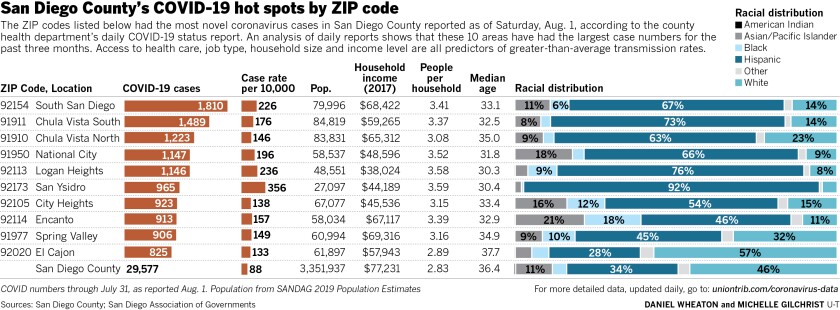
Whether it’s 92154 and 92173 in Otay Mesa and San Ysidro, 91977 and 92020 in Spring Valley and El Cajon or 91911 and 91910 in Chula Vista, many have watched the numbers rise disproportionately in the region’s most diverse communities.
With no vaccine likely this year, many are asking the same question: How will we cool San Diego County’s COVID-19 hot spots?
It is clear that hot weather is not going to do it. As temperatures soared over the weekend, cases continued to arrive, with 529 additional cases and four additional deaths reported Saturday.
While the number of cases recorded in the region’s 10 hardest-hit ZIP codes is not growing as quickly as it was in late April and early May, totals nonetheless climbed at rates from 69 percent to 102 percent in July despite an increased focus on testing and community outreach.
Regardless if it’s 91911 and 91910 in Chula Vista, 92113 and 91950 in Logan Heights and National City or 92114 and 92105 in Encanto and City Heights, it is clear that summer weather has done nothing to burn out these localized COVID-19 contagions.
However, a new, more tailored approach is on the near horizon, and none too soon. No matter what part of the county residents live in, most now know that getting off the governor’s watch list, and getting businesses and schools going this fall will require the current level of activity to subside.
To be sure, much has already been done to tighten the focus on hot spot areas.
Responding to public demands from the mayors of Chula Vista, Imperial Beach and National City in late April, as the number of hospitalizations and deaths started rapidly increasing, the health department opened additional testing locations in disproportionately-impacted areas.
In late June, a regional COVID-19 Taskforce for Equitable Recovery, made up of more than 30 local elected officials, nonprofit leaders, school officials and community organizers held its first meeting with the stated goal of ensuring that underserved communities get the resources needed to survive the effects of the pandemic.
And, less than two weeks ago, the county launched a public health communications campaign to highlight the disproportionate impact of novel coronavirus on the Latino community, noting that while the community is 34 percent of the region’s overall population, it makes up 61 percent of the 29,048 cases, and 45 percent of deaths, detected across the region.
But the ZIP codes where case and death rates have been high for months continue to see growth that makes it clear that there is still work to be done in finding ways to slow the spread.
A small group of community leaders spoke out publicly last week about what they said is a need for new, more culturally-sensitive and targeted outreach effort.
Martin Arias, an executive board member of the San Diego County Hispanic Chamber of Commerce, said he lives in the 92154 area code, the one that has been at the top of the list for months. Moving through the community, he said, he sees situations that look like they must be contributing to the higher number of cases but seem to go relatively unaddressed.
At a transit center near the border, he said, he routinely sees many who likely do not have vehicles of their own waiting to board trolleys and buses.
“Social distancing is not a thing there,” he said. “It is impossible to do.”
Masks and other face coverings may or may not be in use and, here again, resources may not be available to just buy as much as is needed. The places where spread is the greatest tend to be home to higher-than-average concentrations of service-industry workers who are unable to work from home, and statistics show that the 10 ZIP codes with the most cases generally have larger household sizes than the county as a whole. That means it is often more difficult for someone who tests positive to separate themselves from the rest of their household, making it more likely that one infection will turn into two or more.
Combating these issues, Arias and others have argued, requires a bottom-up approach that is difficult for regional or even local governments to fully embrace. Top-down approaches that are not guided by the organizations embedded in communities will simply not be able to achieve the level of trust needed to make progress.
“You have entities that are already embedded in the community like the chamber and so many others; oftentimes, we look past them simply because, you know, they’re not historically the ones we look toward to solve our problems,” Arias said. “I think that they, along with some of our faith-based community leaders, have the most trust in the communities that need to be reached.”
Reached Friday afternoon, Dr. Wilma Wooten, the county’s public health officer and public health director, said that while she is proud of the steps already taken to focus resources south and east, efforts with a deeper cultural focus that embrace the community’s capabilities have been in the planning stages for weeks or months and will soon be visible in the most impacted areas.
“Health equity is important to us,” Wooten said. “We’re trying to represent and have access for everyone.”
County Supervisor Greg Cox, whose district encompasses most of South County, noted in an email that the board will hear a proposal for increased COVID-19 testing at the border in addition to the other initiatives already underway. Like Wooten, he said he understands the current call for better collaboration with local organizations.
“We realize community organizations play a vital role in outreach to residents and for that reason we will be forging partnerships with them to serve as trusted messengers to get this information out to the community,” Cox said.
Investigating and tracing
Last week, Shane Harris, founder of the civil rights organization People’s Alliance for Justice, spoke out loudly about the makeup of the county’s case investigation and contact tracing workforce, noting that while just 25 percent of such workers were Latino, nearly two-thirds of cases were in that demographic group.
He and others keyed on those statistics as evidence that not enough is being done to recruit and employ the kinds of workers who will best be able to effectively interview those who test positive and convince them to take the steps necessary to break chains of person-to-person transmission.
“This is humiliating; this is embarrassing,” Harris said Thursday.
Wooten and a few of her key employees took the time to push back Friday afternoon on the notion that their hiring process, which has more than doubled the number of such workers in recent months and seeks to hire hundreds more, has been blind to cultural sensitivities.
Wooten noted that the county sent its job notice to a broad range of local organizations and not only those that represent various racial and ethnic groups, but also veterans, those with disabilities, American Indians and LGBTQ residents.
“We try to recruit a very diverse group of individuals, and we think we achieved that with over 4,800 applicants,” she said.
Why, then, isn’t there a larger concentration of Latino workers involved in contact tracing and case investigation? Wooten said that in the early going, the county drew from existing employees and temporary nurses to bolster its numbers as quickly as possible. Case investigators, which do initial interviews of each local resident who tests positive, she added, must have a medical background, so racial identity is not the main qualification for who gets hired.
Jeff Johnson, chief of the county’s epidemiology and immunization services branch, said it is difficult to let demographics drive the investigation process because the vast majority of new case notifications that arrive at the county from labs across the region do not include such information. When language barriers are detected, he added, all workers have immediate access to translators. And, when it comes time for contact tracers to interview the close contacts of people who test positive, he said, efforts are made to assign workers who speak the same language if the language is known at time of assignment.
But Wooten added that she is under no illusions that extra effort is required to reach those who may not feel comfortable speaking over the phone with a government official. More than six weeks ago, she said, the county signed a contract with San Diego State University to recruit and train a group of “promotoras” drawn from the communities that are hardest hit. This group, according to the county, includes eight Arabic speakers, six of African American backgrounds and 17 who speak Spanish.
The promotora idea is to work with people who already have a high level of trust in impacted communities. This workforce, she said, is expected to begin its work Monday, visiting those who tracers and investigators have had difficulty reaching over the phone. These workers, Johnson added, will be employed in situations where outbreaks are detected in locations such as apartment complexes. Promotoras will be able to be the trusted faces that go door-to-door and share advice on how to avoid becoming infected.
Outreach
Plans are also in the works to embrace the knowledge of local groups that serve local communities.
On Friday, the county released a request for proposals, asking for applications from community organizations that believe they can provide “community health workers” defined as “trusted” people with “an unusually close understanding of the community served” who can serve as a liaisons to “improve the quality of service delivery.”
The request indicates that the county intends to ink contracts with four such organizations able to provide community health workers well connected to Latinos, African Americans, Asians and Pacific Islanders and refugees.
The program, said Tim McClain, a county communications officer, has been in development for weeks.
“It takes a while to procure these things, to get them ready to go out to bid,” he said. “You can’t tell people about these things in advance, because then you’ve colored the water and then they can’t bid because then they have an unfair advantage.”
Wooten said that she has never been confused about the value of working directly with community organizations. But some efforts, such as testing, needed to have immediate focus as the public health department does the core work of making sure new cases are detected and responded to through isolation and quarantine.
“Community-based organizations are on the ground,” Wooten said. “They are the front-line workers within their communities.”
She added that no one needs to wait for a county contract to reach out to their constituents.
“There is a role for everybody to play, and if someone has a great idea, they should let us know about it and work that idea,” Wooten said.
Hotels
Since March, the county health department has worked with local hotels to house those who need to be isolated or to quarantine after they test positive or are exposed to someone who tests positive for novel coronavirus infection.
But, though the county has had 1,000 or more hotel rooms on contract for months, the number of people using those rooms has regularly been much lower. Friday’s COVID report showed that an average of just 59 public health beds were in use over the past seven days.
This has been a bit of a pet issue for Harris, who said he has been calling for months to find ways to increase the number of people availing themselves of the opportunity to remain separate from their families. When he personally contracted a COVID-19 infection in early March, Harris said, he isolated himself in a county-provided hotel room to avoid infecting roommates and family members at home.
Harris said he does not recall being informed of hotel room availability when he was interviewed by a case investigator after testing positive and said that many he meets in the community are not getting the message. This is particularly important, he added, in communities with what he calls “compacted households” where many roommates or multiple generations of family members share a roof.
Dr. Denise Foster, the county’s chief nursing officer, said that it is standard procedure to ask each person interviewed whether they feel they can safely isolate or quarantine themselves away from others for 10 to 14 days or more. Those who say no, she said, are offered a hotel room.
Why then, are so few of the county’s contracted rooms filling as the number of cases increases? Foster said many are simply more comfortable going through the ordeal near people they know.
“While we are able to check on people, it’s not the same as having someone around who truly is your friend or family member,” Foster said.
She added that the county has tried to accommodate families where possible in order to make it more likely that an infected person in a multi-generational household will be able to opt for a hotel room rather than staying in their residence.
In one case, she said, a homeless man who needed to isolate himself due to a coronavirus infection kept leaving his assigned hotel room for unclear reasons. He was discovered, she said, at the humane society.
“He just wanted his dog, so when we were able to bring the dog in the hotel, he was compliant with staying and successfully isolated through it,” she said.
To put further emphasis on getting those in the hardest-hit ZIP codes to avail themselves of hotel rooms more often, Foster said she believes that the county is doing what it can, working with health care providers in the most impacted areas to get referrals after individuals test positive.
Harris, though, said Thursday that he believes hotels would be more used if those offering them were better known by the people in need.
“They’re not calling the county, because people in our community don’t trust the government,” Harris said. “They trust us, and if we say we have hotel rooms available, I bet you that we would have 100 phone calls tomorrow, saying ‘where’s that hotel room? My cousin tested positive. We need a hotel room.”
The county is due to give its regular bi-weekly COVID-19 update to the full board of supervisors at its next regular meeting Tuesday.



