Food and Common Childhood Illnesses
This is a guest post by Sheila Kilbane, MD, a board-certified integrative pediatrician who practices in Charlotte, NC. Her brand new book Healthy Kids, Happy Moms: A Step-by-Step Guide to Improving Many Common Childhood Illnesses is being released today! You can connect with Dr. Kilbane at SheilaKilbane.com or on Facebook and Instagram.
There are five main triggers of inflammation in your body: food, environmental allergies, environmental toxins, infectious diseases, and stress. Eleven foods cause 90% of our food sensitivities, so it’s often necessary to make modifications to both your child’s diet and environment to help alleviate unwanted symptoms. As an Integrative Pediatrician, I look at not only why the body is responding to a trigger, but also what that trigger is.
Today Lisa asked me to share some specific examples and excerpts from my new book (out today!), Healthy Kids, Happy Moms: A Step-by-Step Guide to Improving Many Common Childhood Illnesses to further explain my approach and how it can help a child in your life.
Helping a Child with a Persistent Cough, Runny Nose, and Wheezing
Gary was four years old when his mother brought him to my Integrative Pediatric Office. He’d had a persistent cough for several months. Throughout the past two years, he’d suffered from recurrent bouts of cough, runny nose, and wheezing that required an Albuterol inhaler. For the wheezing, he’d taken one course of oral steroids, which he did not tolerate. His behavior became erratic, with irritability, mood swings, and sleep troubles.
At that point, his mother knew she never wanted him to take oral steroids again. She decided to switch to an integrative pediatrician (me). Her rationale was that the conventional medical approach aimed to control his symptoms, while her intuition was telling her his chronic cough and congestion had some underlying cause that wasn’t being addressed.
Gary’s mother and I combed through his history. Besides the symptoms above, as an infant, he was extremely fussy and colicky. During the office visit, I observed he was a mouth breather, had a runny nose and dark, puffy circles under his eyes, and his breathing was audible (which I affectionately call “Darth Vader breathing”). Together, these signs pointed to uncontrolled systemic inflammation.
Systemic Inflammation? What’s That?
When most of us think of inflammation, we see images of a hot, puffy, red, irritated, and painful body part, like when a cut gets infected. However, inflammation is more than an acute response to injury, and it’s not localized to one part of our body. Inflammation is an intricate and complex response by the whole body to what it perceives as a threat.
This means the body can have an inflammatory response for many reasons—not just from infection, but also from irritants, allergies (food and environmental), and even stress (physical and emotional).
If we think of inflammation as the body’s self-protection mode, we can understand how and why inflammation can become chronic and spread throughout the body.
To some extent, we need inflammation. If we cut a finger, we need the inflammatory process in that area to stop the bleeding. If we sprain an ankle, we need white blood cells to go to that area and repair the damaged tissues. But when inflammation goes unchecked, the body keeps mounting an inflammatory response to the same trigger, and this leads to chronic inflammation and disease. Integrative medicine teaches us that we need to look not only at why the body is responding to a trigger, but also at what that trigger is.
A Helpful Inflammation Analogy
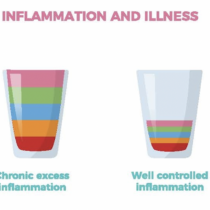
Think of a glass of water. The glass is the body, and the water is the inflammation in the body. Our bodies have a baseline level of inflammation, depending upon the five contributing factors to inflammation: food, environmental allergies, environmental toxins, infectious diseases, and stress.
But a child—let’s call him Solomon—who has several of the common chronic and recurrent childhood illnesses including eczema, asthma, environmental allergies to tree pollen and grasses, chronic runny nose, recurrent ear infections, and constipation, and who eats the standard American diet (SAD) (processed foods with high sugar content and artificial dyes), has a significant amount of systemic inflammation.
Solomon’s glass of water is overflowing with inflammation, preventing his immune system from working optimally.
Since we can’t cut down all the trees and dig up all the grasses, we look at the aspect of Solomon’s environment that we have the most control over: food. We minimize his processed and packaged foods; add in more vegetables, healthy fats, and proteins; replace high-sugar drinks with water; and potentially, gradually remove dairy from his diet.
As we decrease systemic inflammation, the water in the glass will go from overflowing down to half full. Then, when spring and fall allergy seasons come along, or Solomon is exposed to a virus, his inflammation goes up, and maybe the glass fills up again, but it only gets to three-fourths full. Suddenly, he may get through allergy season with little to no allergy medication. He may not need his Albuterol rescue inhaler as much as he did the previous season. And possibly, the laxative he’s been taking for two years is no longer needed.
The higher the amount of baseline inflammation, the longer it may take to get the inflammation under control. Sometimes this means adding more medications or supplements at first, to treat the child’s illness and to strengthen his or her immune system.
Sounds simple, right?
The concept of inflammation and illness is simple, but the body and all of its moving parts are complex. We also have to consider all the other aspects of a child’s environment in order to bring their systemic inflammation to a minimum. I break it down into five main triggers of inflammation to keep the concept as simple as possible. I listed the five triggers in the chart below and they are: food, environmental allergies, environmental toxins, infectious diseases, and stress.
The Causes of Gary’s Inflammation
After a thorough discussion of Gary’s medical history, I examined the inside of his nose. His nasal mucosa was pale, almost bluish, and swollen shut, so he had to breathe through his mouth.
Environmental allergies often cause the nasal mucosa to be pale and swollen. When I was first out of residency, I used medications to treat the symptoms of patients like Gary. I would have prescribed an inhaled steroid for him, along with an antihistamine for allergies, a topical steroid for the eczema, and a nasal steroid spray for the nasal congestion. This would have addressed most of his inflammatory symptoms during the time of year when his allergies and asthma flared. On top of that, if he had constipation, I would have also given him a laxative.
When I know a child has an increased risk of asthma or any other type of inflammatory issue like allergies, constipation, or reflux, I now look at the bigger picture and ask, How can I reduce this child’s overall systemic inflammation and improve all of his symptoms, not just one of them?
As luck would have it, Gary’s previous pediatrician had done allergy testing through blood work and discovered a severe dust mite allergy. My first question when a child has a dust mite allergy is: How old are his mattress and pillows?
Mattresses and pillows are dust mite havens. One study, conducted at a London hospital, found that up to a third of a pillow’s weight could comprise bugs, dead skin, and dust mites.
Gary was sleeping on a fifteen-year-old mattress from his uncle’s college days. Given the severity of his dust mite allergy, his mother and I decided they should invest in a new mattress. I also recommended new pillows and putting plastic dust mite covers over the new mattress and pillows to prevent the critters from settling into them again. These covers would help us keep Gary’s dust mite exposure to a minimum while he slept.
Was Dairy a Problem?
I recognized after years of practicing integrative medicine that Gary’s symptoms were classic for a dairy sensitivity. So we removed it from his diet for three weeks.
A selective elimination diet (which is what we did with Gary), is the gold standard test to determine a food sensitivity.
A Quick Turnaround
At Gary’s follow-up appointment three weeks later, his chronic nasal congestion and cough had almost completely resolved. Eventually, the dark circles under his eyes disappeared, as did his mouth breathing, and his need for Albuterol decreased. Since Gary had such significant improvements, we kept dairy out of his diet as a new lifestyle.
Gary improved rapidly, and to this day, he is doing great. I believe we changed the course of his health for the better, in both the short and long term. He is one of the hundreds of children I have seen over the years who have enjoyed an improved path with their wheezing or asthma after we methodically worked to decrease their systemic inflammation.
I’ve heard this question many times from parents: Why didn’t anybody tell us this before (with regard to food and systemic inflammation)? My response is always the same: When I trained, nutrition wasn’t part of the curriculum. I had no way of looking at food as a potential source of inflammation. It wasn’t even on my radar. If I’d seen your child before I started studying about nutrition and integrative medicine, I would have given you the same advice your previous pediatrician gave you.
Gary’s situation was straightforward. The nasal congestion, dark circles under his eyes, and his Darth Vader breathing are easy to identify in kids and adults when you know what you are looking for. But some cases are more complex and require further probing.
Food Allergies versus Food Sensitivities
Food allergy tests look for allergens that can trigger a powerful, profound, and fast inflammatory response and can lead to hives, lip swelling, coughing, wheezing, vomiting, and trouble breathing. True food allergies are serious and can be life-threatening. The reaction typically occurs within 15-30 minutes of exposure, or it can be delayed up to 12 hours.
In conventional pediatrics, if we suspect a child has a food allergy, we order skin prick testing or blood work looking for an elevated IgE protein to the particular food in question. If the allergy test is negative, the patient is told to continue eating the food.
Many times over the years, in my initial consultation with a patient, the parents will say, “Oh, she’s already had food allergy testing. She’s not allergic to any foods.” Unfortunately, a negative outcome on an allergy test doesn’t mean the child’s diet isn’t creating inflammation. That’s where an understanding of food sensitivities comes into play. Gary’s case will help us understand more about food sensitivities.
In my experience, it takes about three to six months to decrease systemic inflammation and allow the GI tract (the digestive system) and the immune system to work optimally. Symptoms usually improve within two to four weeks, but to get the long-lasting improvements, we need to keep the food out for several months. After that, the kids often tolerate small amounts of problematic foods like dairy with no significant flare-up of their original symptoms (i.e. runny nose, nasal congestion, cough, mouth breathing).
Food sensitivity tests are in widespread use by integrative and functional medical practitioners, but we are not trained to use them in conventional medicine. You will get a faster answer with food sensitivity testing versus an elimination diet, but when a child’s system is inflamed, such as Gary’s when he initially came to see me, many foods may test positive on one of those tests. Some parents might be overwhelmed by the prospect of trying to remove several foods all at once from a child’s diet. And since we know that eleven foods cause 90% of our food sensitivities (with dairy being at the top of the list), we start with the primary culprit and then do testing if and when it is needed.
When I work with families to first decrease the child’s overall systemic inflammation, we first identify their main triggers of inflammation (such as dairy and dust mites, as with Gary). We make the necessary modifications to their diet and environment and then, if the child is still having symptoms, we may do food sensitivity testing. When working with children, I only recommend you do these tests under the supervision of a doctor or nutritionist trained in integrative or functional medicine.
The complexity of testing for food reactions led me to write an entire chapter in my book on the topic. You can download the reference table I created to help illustrate the different ways we can test for food reactions. There is so much misunderstanding about this for patients and physicians.
The table also has a list of symptoms associated with celiac disease, food intolerance, and histamine intolerance.
Takeaways
- Life comprises a set of complex variables affecting us at all times, including with illness. By breaking down the main triggers of inflammation into an easily understood, organized fashion, you can understand how to gain control of your child’s health.
- The important thing is to be pragmatic and remember that each trigger of inflammation carries equal weight. If we address one area with 100 percent effort but ignore the others, you may not see the true health transformation you’re seeking for your child and perhaps your family.
- Understanding these triggers of inflammation can also help you to partner more easily with your child’s doctor, to find the root of chronic and recurrent inflammatory illnesses more efficiently.
- To learn more about how to improve your child’s health, my book Healthy Kids Happy Moms – 7 Steps to Heal and Prevent Common Childhood Illnesses is now available.
Turmeric Rice
For anyone with food sensitivity or illness, this Turmeric Rice recipe contains tons of anti-inflammatory properties that help your gut heal.
Servings: 4
- 1 cup basmati rice or jasmine, cooked according to package
- 1/2 cup broccoli chopped into small pieces
- 2 1/4 cups water
- 1 1/2 tablespoons coconut oil (or ghee)
- 1 tablespoon turmeric powder more to taste
- 1/4 teaspoon ground black pepper
- sea salt to taste, Himalayan sea salt is preferable
- 4 cardamom seeds 4-6, whole, dried
- 3/4 cup spinach chopped
- raisins a handful (optional)
- 1 cup organic chicken cooked, chopped (optional)
-
Cook rice according to package.
-
Add the broccoli into the rice when there is about 5 minutes left of cooking.
-
Once rice is done, add in all other ingredients and combine well.
- This can be made in a rice cooker or on the stove just as you would cook rice. Follow the instructions on the package for the rice. You may need to add a bit more water than what the rice package indicates.
- Use brown or black rice for a lower glycemic index.
- Although the black pepper facilitates absorption of the turmeric, those with Crohn’s disease or ulcerative colitis should leave out the black pepper, because this allows the turmeric to remain within the GI system and carry out its anti-inflammatory properties where it’s needed most—in the gut.
- We recommend organic ingredients when feasible.